Compliance: practically speaking, it describes the change in pressure when a given volume is delivered to the lungs, eg, when pt is on volume-controlled mechanical ventilation. Compliance = ΔV ÷ ΔP
Compliance (elastic resistance) determines 65% of the work of breathing. If the lung has low compliance, it requires more work from breathing muscles to inflate the lungs.
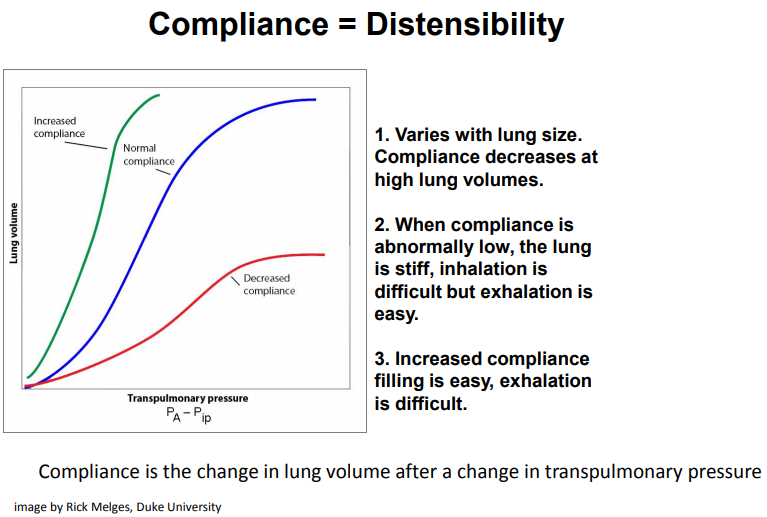
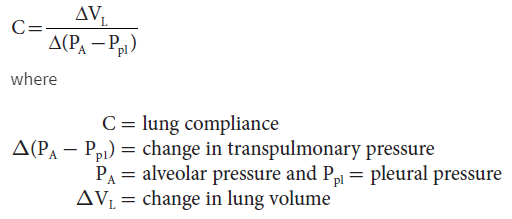
The compliance of a system is defined as the change in volume that occurs per unit change in the pressure of the system. In layman terms, compliance is the ease with which an elastic structure can be stretched (distensibility). Compliance is, therefore, basically a measurement of the elastic resistance of a system. Pulmonary compliance (C) is the total compliance of both lungs, measuring the extent to which the lungs will expand (change in volume of lungs) for each unit increase in the trans-pulmonary pressure (when enough time is allowed for the system to reach equilibrium).
Transpulmonary pressure (mine--distending pressure) is the pressure gradient between the inside alveolar pressure & outside pleural pressure. It mainly measures the force of lung elasticity at each point of respiration (recoil pressure). Alveolar pressure is the air pressure inside the alveoli. Pleural pressure is the pressure of the fluid present inside the space between visceral pleura (layer adhered to lungs) & parietal pleura (chest wall lining layer). Normally the total compliance of both lungs in an adult is about 200 ml/ cm H2O. Physicians rely on this concept to understand some pulmonary pathologies & help guide therapy & adjust ventilator pressure & volume settings.
Source: https://www.ncbi.nlm.nih.gov/books/NBK538324/
The recoil force of the lungs, measured as the transpulmonary pressure, is the difference between the alveolar & pleural pressures.
Alveolar pressure is determined as the pressure at the airway opening (Pao)--i.e., the mouth-- when airflow is arrested & the glottis is open. The pleural pressure is determined indirectly by measuring the pressure in the esophagus using an esophageal balloon catheter.
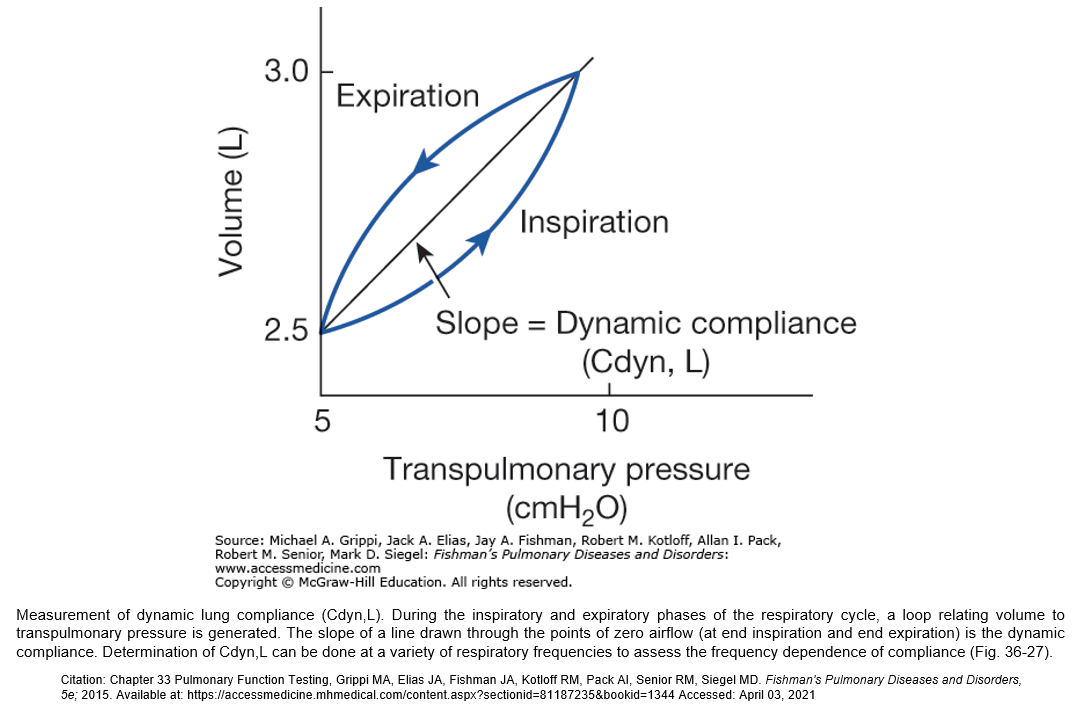
Source: Fishman's Pulmonary Diseases and Disorders. Chapter 33: Pulmonary Function Testing.
Compliance determines 65% of work of breathing. If the lung has low compliance, it requires more work from breathing muscles to inflate the lungs. In specific pathologies, continuous monitoring of the lung compliance curve is useful to understand the progression of the condition & to decide on therapeutic settings needed for ventilator management.
Lungs with low compliance are stiff lungs & will require much greater pressure to reach a given volume compared to lungs that have high compliance. There are several factors that affect lung compliance including alterations in the ribs (ie. fractures), ossification of the costal cartilage, obesity, muscular or neural changes to intercostal muscles (ie. paralysis or strain/pain), position (prone/supine), structural abnormalities (ie. kyphosis or scoliosis), increased intraabdominal pressure, & age.
Compliance is the opposite of elasticity, & elasticity is the tendency of lung tissue to return to its original (or relaxed) position after an applied force has been removed.
Normal chest wall compliance in adults is approximately 100-200 ml/cm H2O. However, children have far lower chest wall compliance at 2.5-5.0 ml/cm H2O.
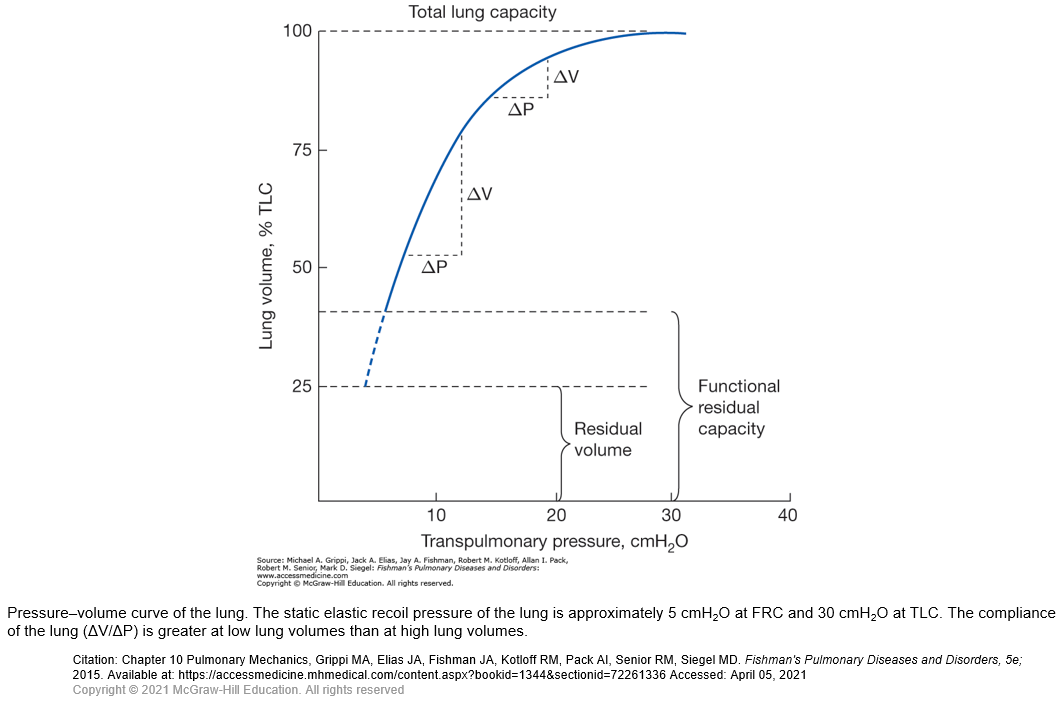
Another way to determine compliance is graphically using a pressure volume curve. The slope of the line in the is equal to the lung compliance.
Source: https://www.openanesthesia.org/chest_wall_compliance_calculation/
During spontaneous ventilation, the total compliance of the respiratory system, including the chest wall & the lung, is 100 ml/cmH2O. The lung compliance is around 200 ml/cmH2O. In anesthetized ventilated normal individuals, the total compliance of the respiratory system is slightly decreased (70–80 ml/cmH2O). Source: Lu, Q, et al. Measurement of pressure–volume curves in patients on mechanical ventilation: methods and significance. Crit Care 2000, 4:91–100.
In patients with acute respiratory failure, determination of lower & upper inflection points and measurement of respiratory compliance should become a part of the routine assessment of lung injury severity, allowing a bedside monitoring of the evolution of the lung disease & an optimization of mechanical ventilation.
The static pressure–volume curves are impaired in acute respiratory distress syndrome (ARDS). Three abnormalities are characteristic [1]: the appearance of an initial inflection point, which corresponds to the opening pressure of the collapsed bronchoalveolar zones; reduction of the slope of the ascending limb, which indicates the loss of lung aeration that characterizes acute lung injury [2]; and lowering of the volume that corresponds to the upper inflection point, which increases the risk of mechanical ventilationinduced over-distension [3]. The lower inflection point determines the minimal level of PEEP at which alveolar recruitment starts. The upper inflection point determines the pressure level that is not to be exceeded in order to avoid barotrauma and/or ventilator-associated lung injury.
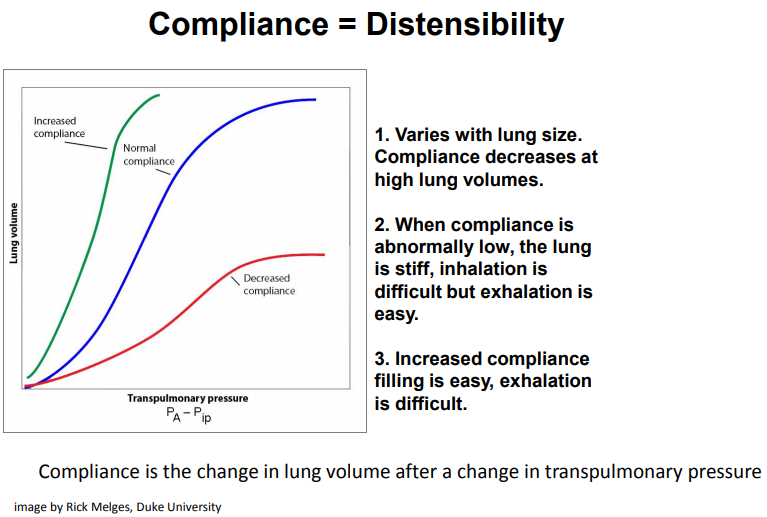
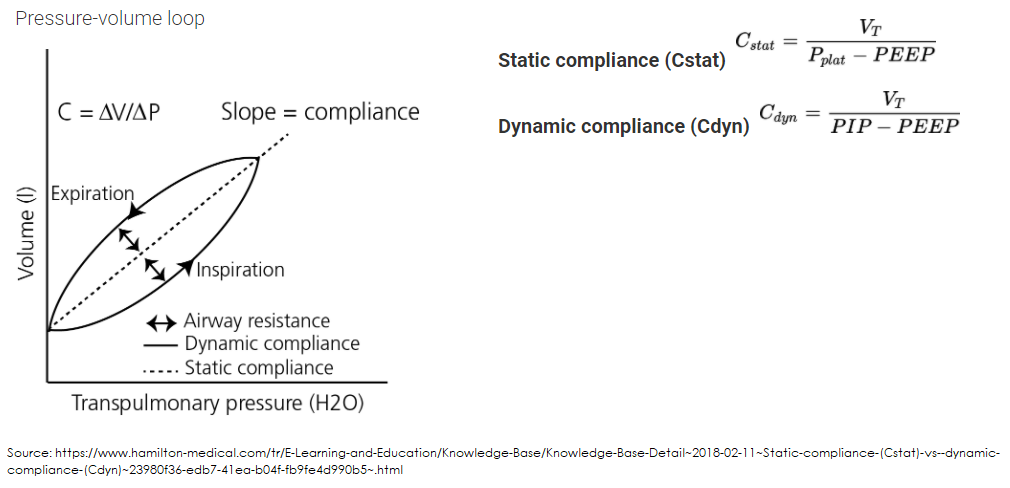
Dynamic Compliance: = TV/(PIP - PEEP); affected by secretions, coughing, etc. Normally 50 -100 mL/cmH2O
(compliance during breathing -- where airflow resistance becomes a factor)
Dynamic compliance is change in volume divided by change in pressure, measured in the presence of gas flow. In essence, it is the same compliance but measured during normal inspiration & expiration.
Static Compliance: = TV/(Pplat- PEEP); want this > 30; typically it'll be 30-60 mL/cmH2O; if compliance is falling, think ARDS developing
Note: for pneumothorax, since air is leaking into thoracic cavity and compressing the alveoli from the outside, the alveolar (Static) compliance will decrease; the dynamic compliance will also decrease because Dynamic Compliance encompasses airways (ie, ETT, trache, bronchi) AND alveoli.
Video: Respiratory Therapy - Another breakdown of Dynamic vs Static Compliance by Respiratory Coach
Video: https://www.youtube.com/watch?v=61pmJWt50-M -- RT Clinic: Basics of Plateau Pressure and Static Compliance, Early Indicators of ARDS -- Jimmy McKanna
Analysis of volume-dependent dynamic compliance showed that for keeping the lung open during ventilation, PEEP could be set 5 cm H2O lower than LIP.
Traditionally 3 distinct features of the static pressure-volume (PV) loop of the respiratory system are used to assess the mechanical stress imposed by artificial ventilation to the lung. The lower inflection point (LIP) of the inspiratory limb of the PV loop is thought to indicate the pressure at which the majority of lung units are recruited. The upper inflection point (UIP) indicates the pressure at which overdistention starts. The linear steep segment of the PV curve between LIP and UIP is assumed to indicate the zone between and expiratory collapse and overdistention, although there is evidence that reinflation of collapsed lung units continues above LIP and throughout the linear part of the PV loop and perhaps even above UIP. Hence it is hoped that lung injury from both shear stress and overdistention is avoided when tidal ventilation occurs on the linear segment of the PV curve between LIP and UIP. This concept is intuitively appealing & it may improve ventilatory support in patients. Recent studies have challenged these concepts, however, as the mechanical properties of the respiratory system may depend on the PV history of the current tidal ventilation. The assumption that information obtained from static maneuvers like the PV loop can be applied to tidal ventilation may be incorrect, given the pronounced differences in pressure volume history. Rather than studying the respiratory system under artificial conditions, we have assessed dynamic mechanics during uninterrupted ventilation & hence without affecting the actual pressure volume history of the lung. We analyzed compliance within the tidal breath, taking into account the endotracheal tube related flow-dependent resistance.
Source: https://pubmed.ncbi.nlm.nih.gov/11064617/ Static versus dynamic respiratory mechanics for setting the ventilator
Obviously, when you pump gas into a person's chest, the pressure-volume relationship is going to be a complex combination of several factors. Of these, the dominant players will be the chest wall and the tissues of the lung itself. When asked to describe this concept, one would likely be expected to regurgitate this equation:

Where, predictably, CRS is the compliance of the respiratory system as a whole, CL is the compliance of the lung and CCW is the compliance of the chest wall. Usually, textbooks give normal values for these compliances; for the lung and chest wall, these are 200ml/cm H2O.
The compliance of the lungs and chest wall are related to the elastic properties of these structures.
Source: https://derangedphysiology.com/main/cicm-primary-exam/required-reading/respiratory-system/Chapter%20031/static-dynamic-and-specific-compliance
Compliance Curve Problems: Mechanical Ventilation
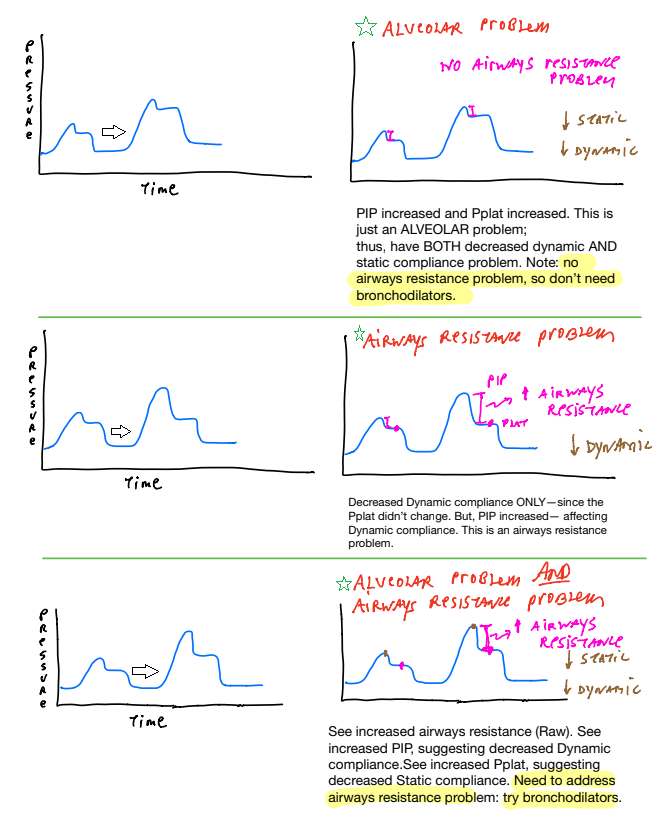 here. . . PIP >> Pplat = resistance issue
here. . . PIP >> Pplat = resistance issue
Video: Dynamic vs Static Compliance with Graphics Analysis!
Compliance
“Quasi-static” Compliance = VT/Pplat – PEEPtotal
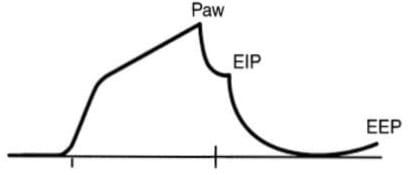 Source: https://litfl.com/pulmonary-mechanics/
Source: https://litfl.com/pulmonary-mechanics/
The terms compliance, distension, & distensibility may seem synonymous, but clinically their meanings can be quite different. One easy analogy may help. A new rubber balloon is distensible (expandable with gas or liquid) and it also is compliant (its rubber walls resist inflation & assist deflation). A plastic bag from the grocery store is distensible, but it is not compliant. A rubber balloon that is filled and then forgotten will remain distensible but become less compliant as its walls lose their elasticity. Certain diseases affect lungs in such fashion, notably emphysema in which lung elasticity is reduced by proteases released into the alveolar parenchyma by resident macrophages and recruited neutrophils. Lungs of patients with severe emphysema can be inflated but may retain gas even during a pneumothorax. Source: https://thoracickey.com/surfactant-biology-and-lung-compliance/
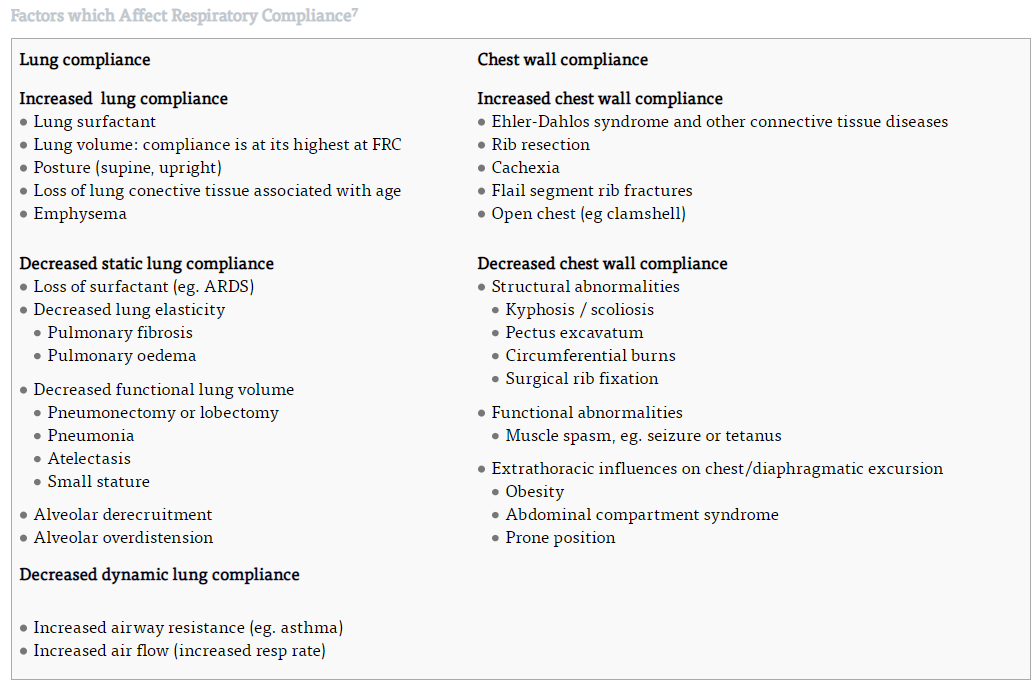
Factors Affecting Pulmonary Compliance
Elastic Property of the Lung Tissue: These result from the collagen & elastin fibers meshed inside the lung parenchyma. When the lung is outside the body system & in a deflated state, these fibers fully contract due to elasticity. When the lung expands, they elongate and exert even more elastic force, similar to a rubber band. Thus the flexibility of these fibers determines the compliance of the lungs. They could be damaged or affected by specific pulmonary pathologies.
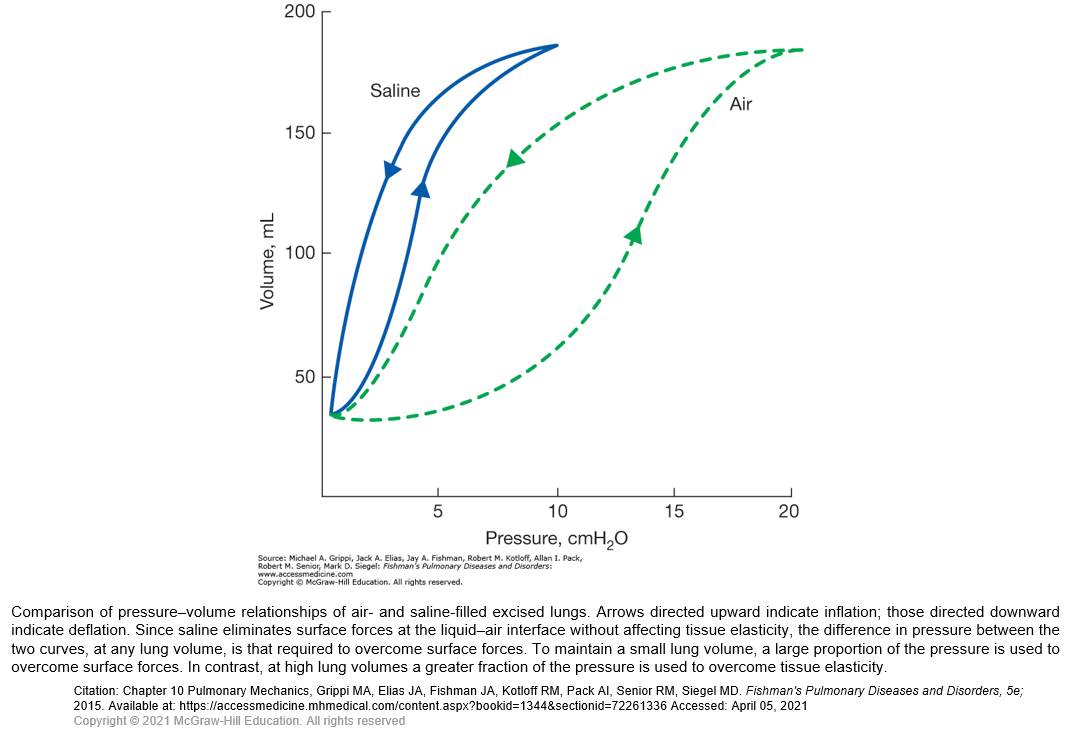
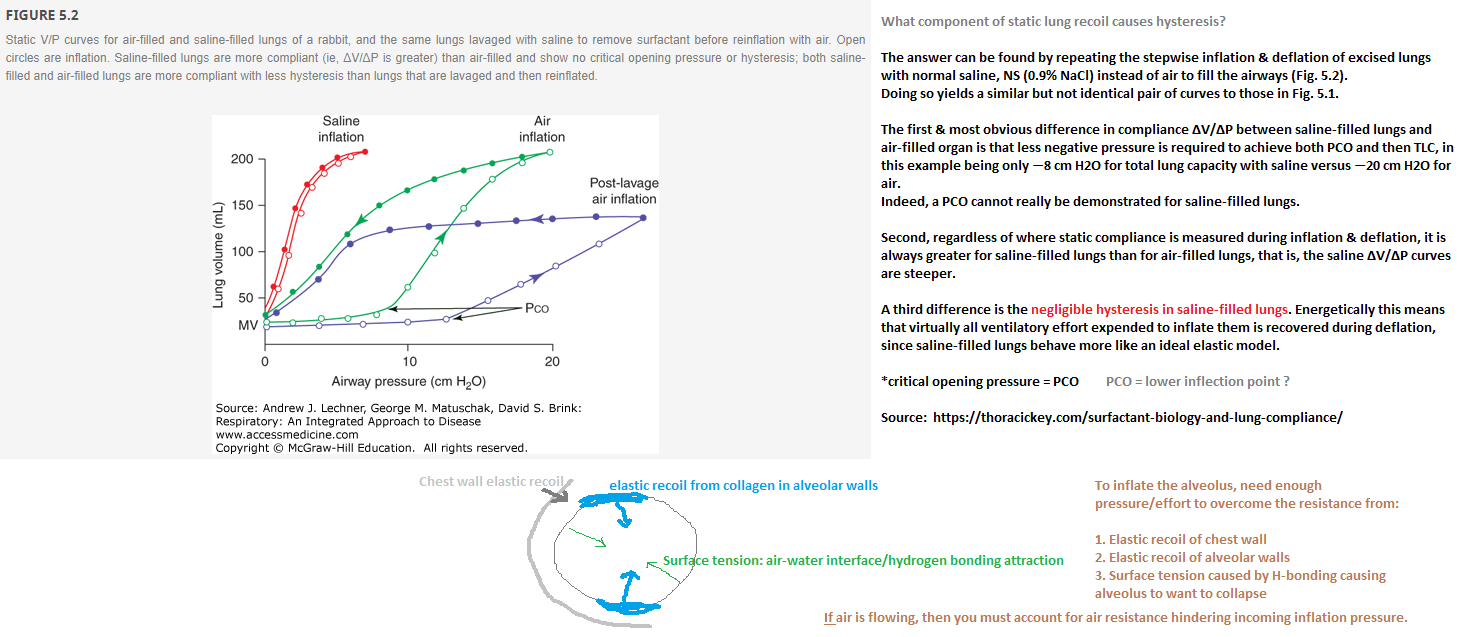
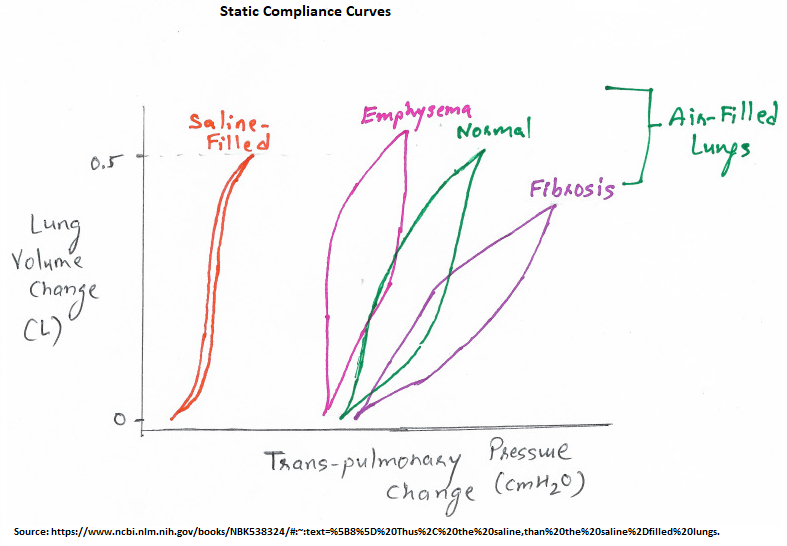
Surface Tension Elastic Force: One of the important concepts affecting lung compliance is the elastic property of the lung contributed to by the surface tension of the alveolar lining. There is a compliance difference between saline-filled and normal air-filled lungs. Air-filled lungs work as a different elastic structure inside the pulmonary system. Its flexible property is not only determined by the elastic forces of the tissue but also contributed to through surface tension exerted by the fluids lining the walls of the alveoli. When water forms a surface with air, the water molecules demonstrate strong, attractive forces for one another, causing contraction of the surface. This principle is what holds a raindrop together.
Similarly, water lining the inner surface of the alveoli attempt to force air out of the alveoli and tries to collapse it. This force is the surface tension elastic force. Its minimum value is 35 to 41 dyne/cm. Thus, the saline-filled lung has higher compliance than the normal air-filled lung, since the pressure required to expand the air-filled lung is higher than the saline-filled lungs. [mine. . .because a saline-field alveolus has no air-water interface. . .]
Surfactant: If you measure the alveolar pressure using surface tension exerted by the lining fluid based on the Laplace law: Pressure = 2 x T (Surface Tension) / R (Radius), one notes that the pressure within the smaller alveoli would be higher than the pressure within large alveoli which will collapse the small alveoli. However, in a typical scenario, this doesn't happen. It occurs where surfactants play a role.[9] A surfactant is a surface-active agent in the fluid, secreted by type II alveolar epithelial cells lining the alveoli. It is a complex molecule containing phospholipid dipalmitoylphosphatidylcholine, surfactant apoproteins, and calcium ions. They reduce the surface tension by partial dissolution. Now returning to the mechanics, the smaller alveoli have a small surface area, which leads to a higher concentration of the surfactants and eventually lower surface tension.[10] Due to its role in surface tension modification, it indirectly affects the compliance of the lung.
Lung Volume: Compliance is related to the lung volume, considering the formula relating volume and pressure. However, to eliminate this variable, specific compliance is measured using the formula: Specific Compliance = Compliance/ FRC (Functional Residual Capacity).
Age: This factor minimally influences compliance. Pulmonary compliance increases with age are owing to the structural changes in the lung elastin fibers.
A minimal volume of air does remain in the lungs because of closure of small airways resulting in the trapping of air in more distal airspaces.
The P–V curve consists of 3 segments: (1) An initial flat segment that reflects a very low compliance, indicating collapse of peripheral airways or alveolar units. (2) A segment with a steeper slope; the transition between these two segments, which can be more or less abrupt, is the lower inflection point (LIP). This high & stable compliance over the linear segment following the LIP during inflation may be explained by continuing recruitment. (3) At large volumes & high pressures, the slope decreases & the compliance approaches zero when the respiratory system is distended; the point at which a decrease in compliance can be identified is the upper inflection point (UIP).
Hysteresis occurs because the system is not perfectly elastic; thus, don't see the deflation curve looking exactly like the inflation side of the PV curve.
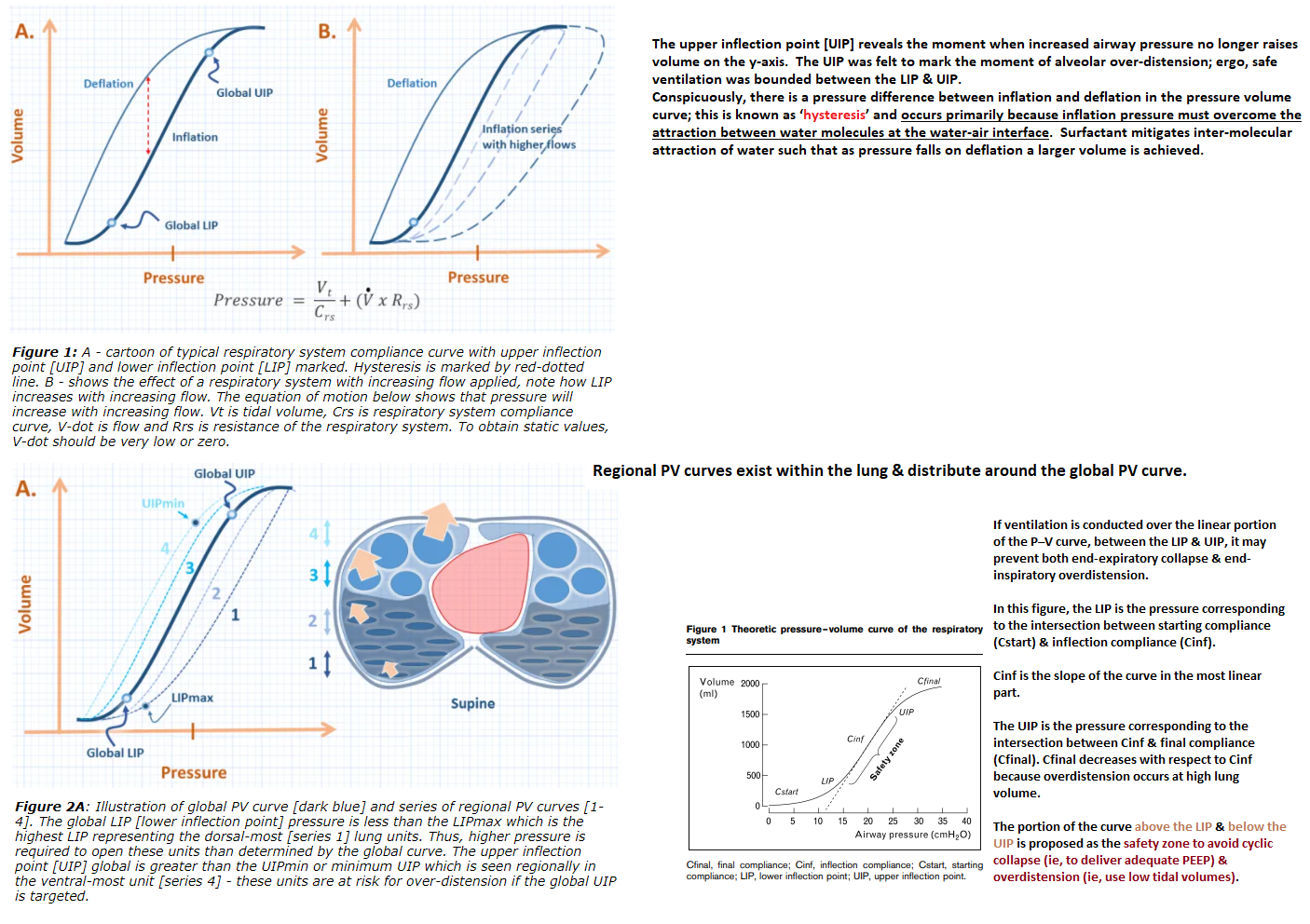
If ventilation is conducted over the linear portion of the P–V curve, between the LIP & UIP, it may prevent both end-expiratory collapse & end-inspiratory overdistension. In this figure, the LIP is the pressure corresponding to the intersection between starting compliance (Cstart) & inflection compliance (Cinf). Cinf is the slope of the curve in the most linear part. The UIP is the pressure corresponding to the intersection between Cinf and final compliance (Cfinal). Cfinal decreases with respect to Cinf because overdistension occurs at high lung volume. The portion of the curve above the LIP & below the UIP is proposed as the safety zone to avoid cyclic collapse (adequate PEEP) & overdistension (low tidal volume).
Source:
Kenney JE. PV Curves in 1000 words
Similar to dynamic compliance, except that static PIP is substituted for PIP. Measure static peak pressure (also called plateau pressure) by occluding the exhalation port at the beginning of exhalation (no flow = static pressure).
Comparing dynamic with static compliance may indicate the type of processes causing changes in the elasticity of the lung. Dynamic compliance is affected by both elasticity and airway resistance. Static compliance reflects elasticity and is not affected by airway resistance because there is no flow.
Dynamic Compliance
Clinical Significance
Certain pulmonary diseases can influence changes in lung compliance. The following are pathologies that can increase or decrease lung compliance:
Emphysema or COPD: In both of these conditions, the elastic recoil property of the lung suffers damage due to a genetic cause (alfa-1 antitrypsin deficiency) or an extrinsic factor (e.g., smoking). Because of poor elastic recoil, such patients have high lung compliance. Their alveolar sacs have a high residual volume, which in turn causes difficulty in exhaling the excess air out of the lung, and patients develop shortness of breath.
Pulmonary Fibrosis: Certain environmental pollutants, chemicals, or infectious agents could cause fibrosis of the lung tissue. Genetic diseases can also do so. In fibrosis, lung elastin fibers are replaced by collagens, which are less elastic & decrease the compliance of lung. Such patients need higher work of breathing to inflate more rigid lung alveoli.
Newborn Respiratory Distress Syndrome: Usually, surfactant secretion begins between the sixth and seventh months of gestation. Premature newborns have little or no surfactant in the alveoli when they are born, and their lungs have a significant tendency to collapse. As described earlier, surfactant helps in reducing surface tension and thereby increases compliance of the lung. An absence of the surfactant leads to a decrease in pulmonary compliance, and this condition is called newborn respiratory distress syndrome. It is fatal and requires aggressive measures by continuous positive pressure breathing.
Atelectasis /ARDS: Atelectasis is the collapse of lung alveoli & usually occurs in the dependent parts of the lungs. Following operative anesthesia, this could be one of the potential complications. In the case of atelectasis, pulmonary compliance decreases due to a decrease in the volume of the lung and requires higher pressure to inflate the alveoli. Obtaining a compliance curve along with oximetry & ABG is one useful method in ICU monitoring.