Video showing relationship between flow-volume & volume-time
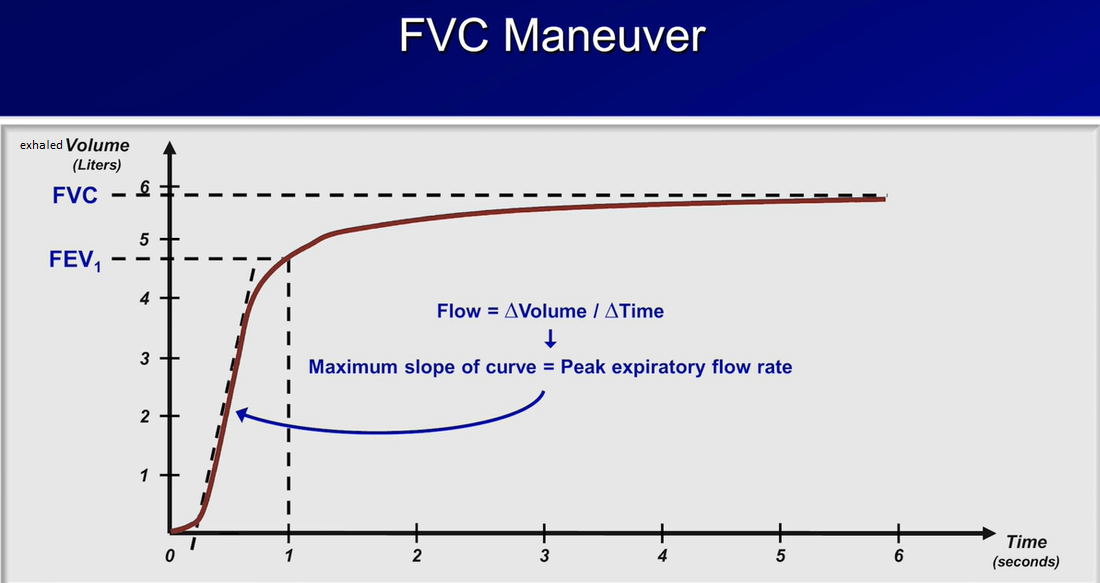
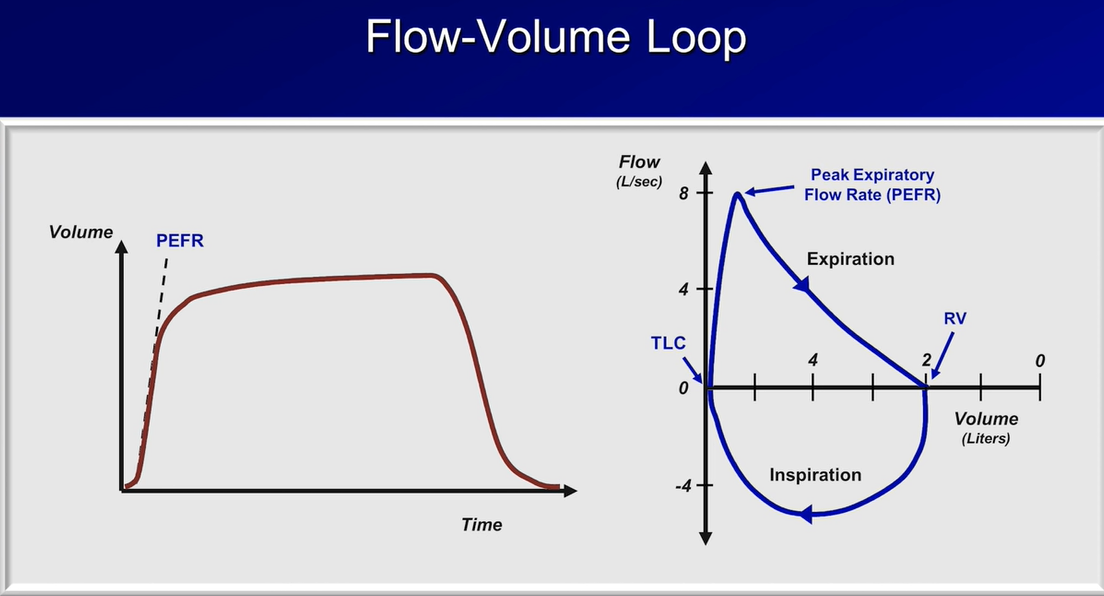
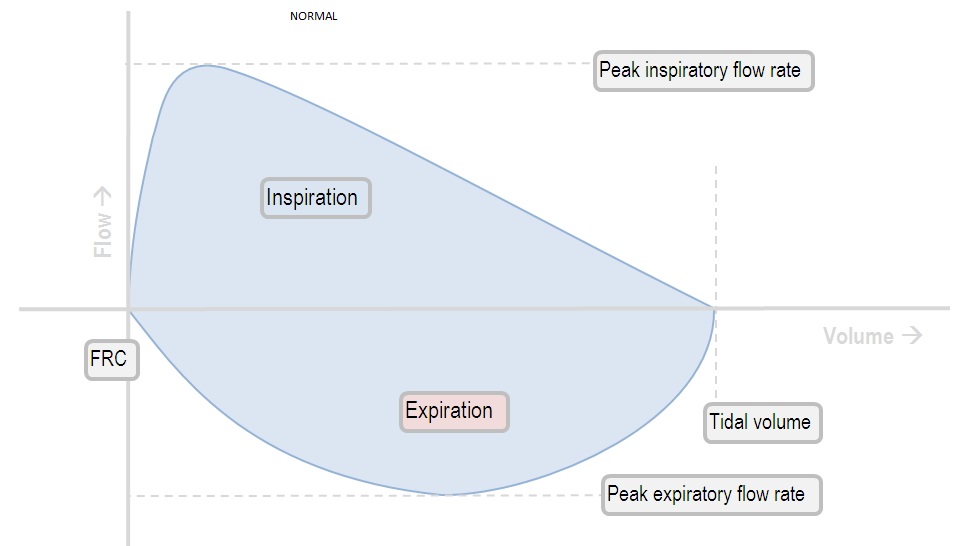
With the classical spirometer, the patient forcibly exhales into the machine; the peak expiratory flow rate & the shape of the expiratory flow-volume curve is therefore the best measure of airway resistance.
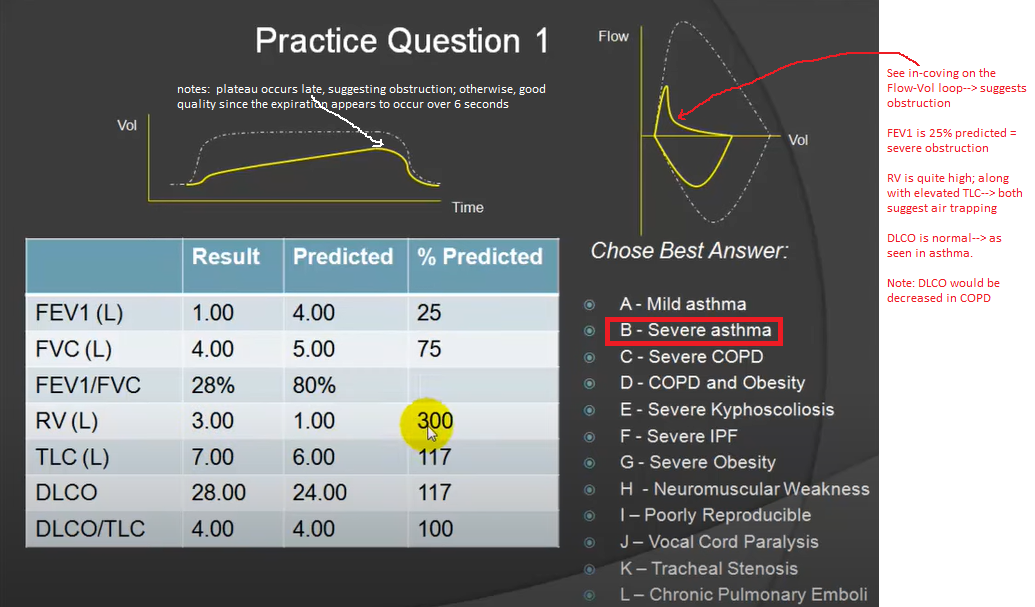
Analyzing flow volume loops provides a quick way to detect lung disease. The appearance of the loop can reveal the presence of obstructive and/or restrictive lung disease.

The location of the airway obstruction can also be identified from the shape of the flow volume loop.

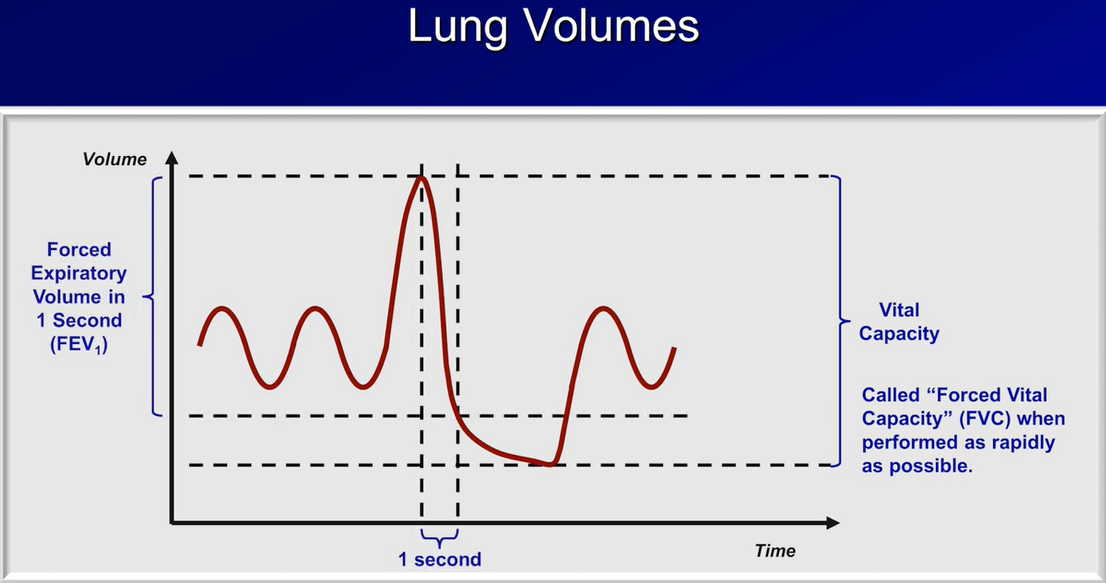
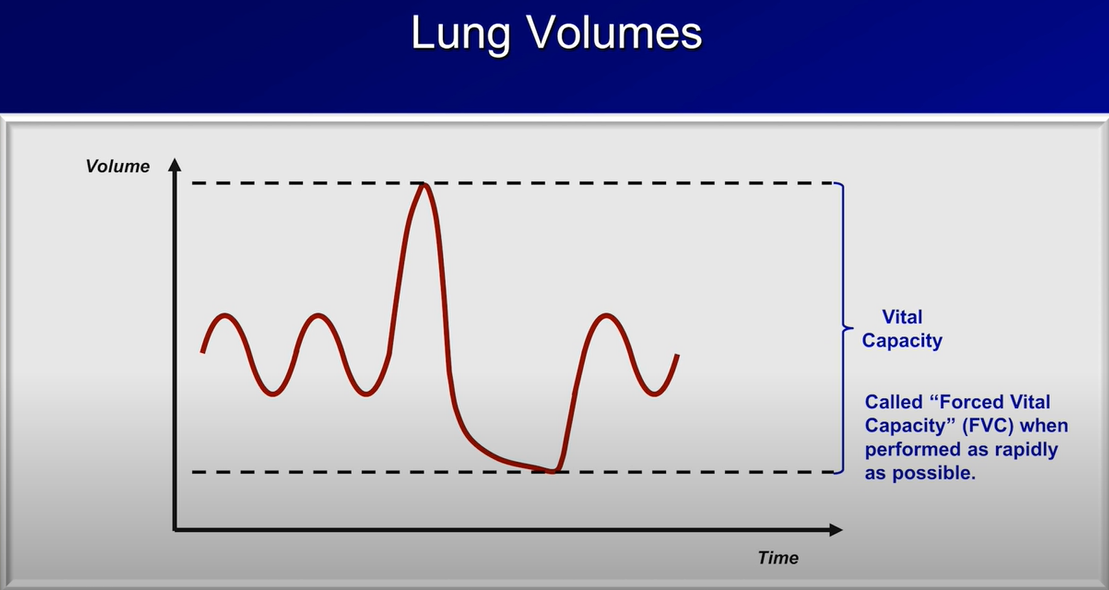
In a spontaneously breathing patient, the flow volume loop is measured using a forced vital capacity maneuver (FVC). The patient is instructed to take a maximum deep breath (to total lung capacity). They then forcefully exhale all of the air out completely (to residual volume). When they can no longer exhale, they take a forceful breath back in to total lung capacity.
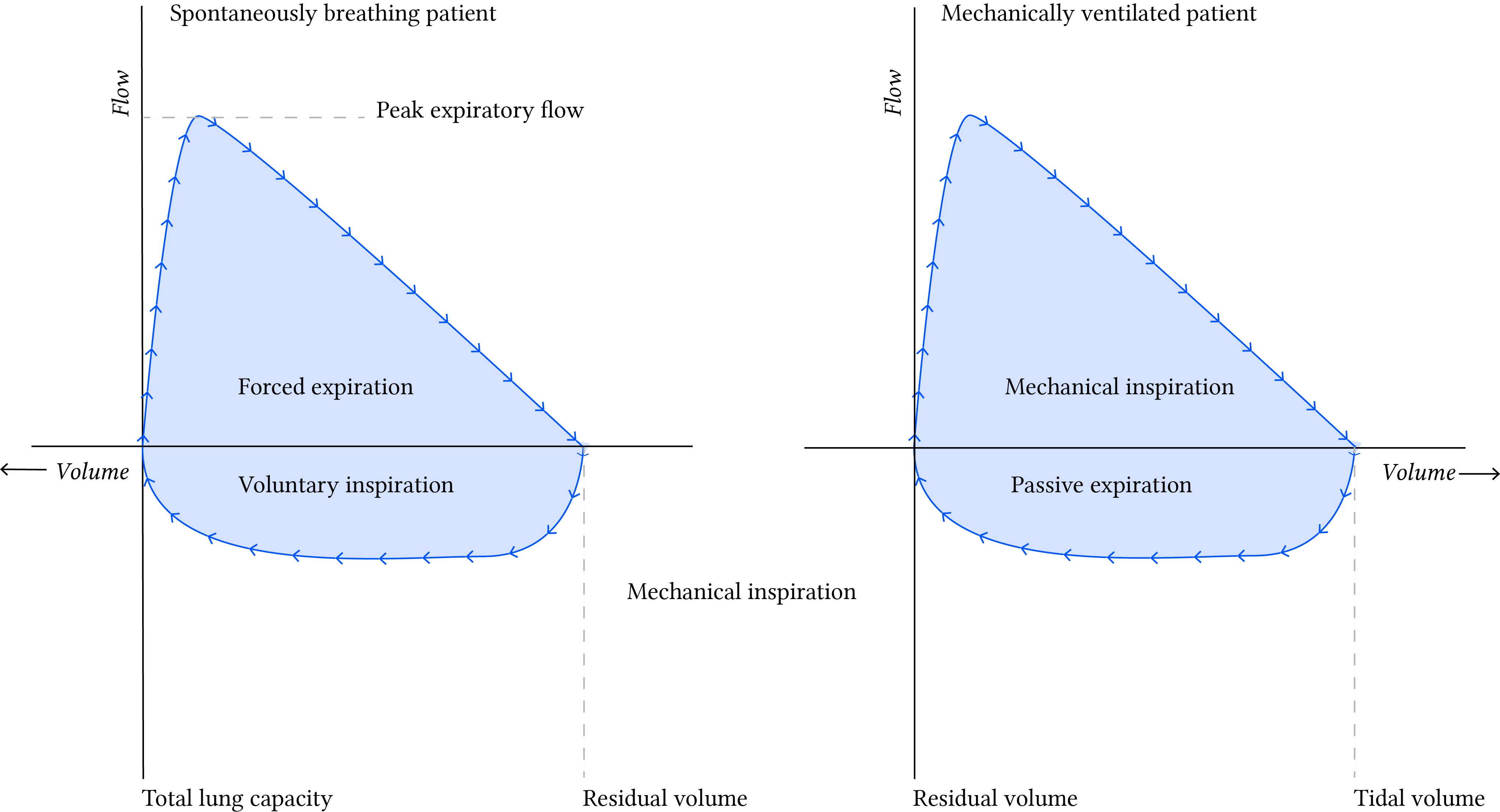
Flow volume loops can also reveal the presence of airway secretions during mechanical ventilation that auscultation alone may miss.
As air passes by secretions in the airway, tiny flow and pressure changes occur. These tiny changes produce a saw tooth pattern during inhalation and exhalation. (the FVC maneuver is not required to detect secretions during mechanical ventilation).

The fundamental difference is in the fact that in the ventilator loop is by convention upside-down, & the volume measurements on the x axis measure in opposite directions. See below:
Sources:
https://respiratorycram.com/flow-volume-loops/
https://derangedphysiology.com/main/cicm-primary-exam/required-reading/respiratory-system/Chapter%20556/interpreting-shape-flow-volume-loop
Videos:
https://www.youtube.com/watch?v=Gr0ZxoZR58Y&t=136s Lung Function Test (Spirometry)
https://www.youtube.com/watch?v=Zs8Fs5HaJHs Taking a Spirometry Test
https://www.youtube.com/watch?v=yJzbiVUL58Y Alia
Physiology practical demonstrations - Spirometry
Pulmonary Function Tests (PFT): Lesson 2 - Spirometry Strong
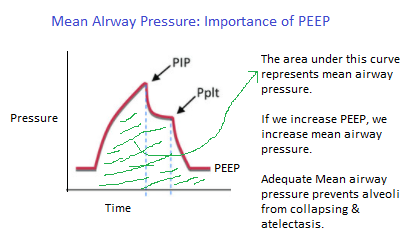
Mean Airway Pressure
PFT tips:
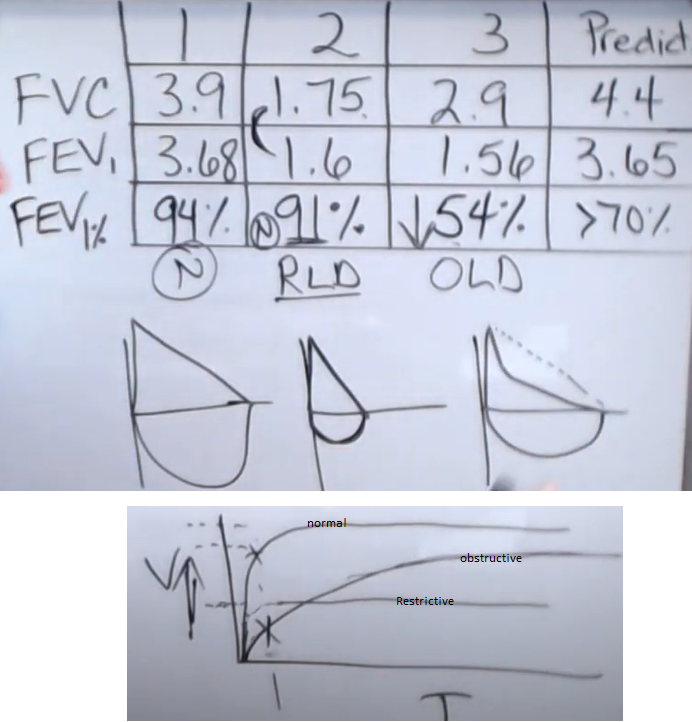
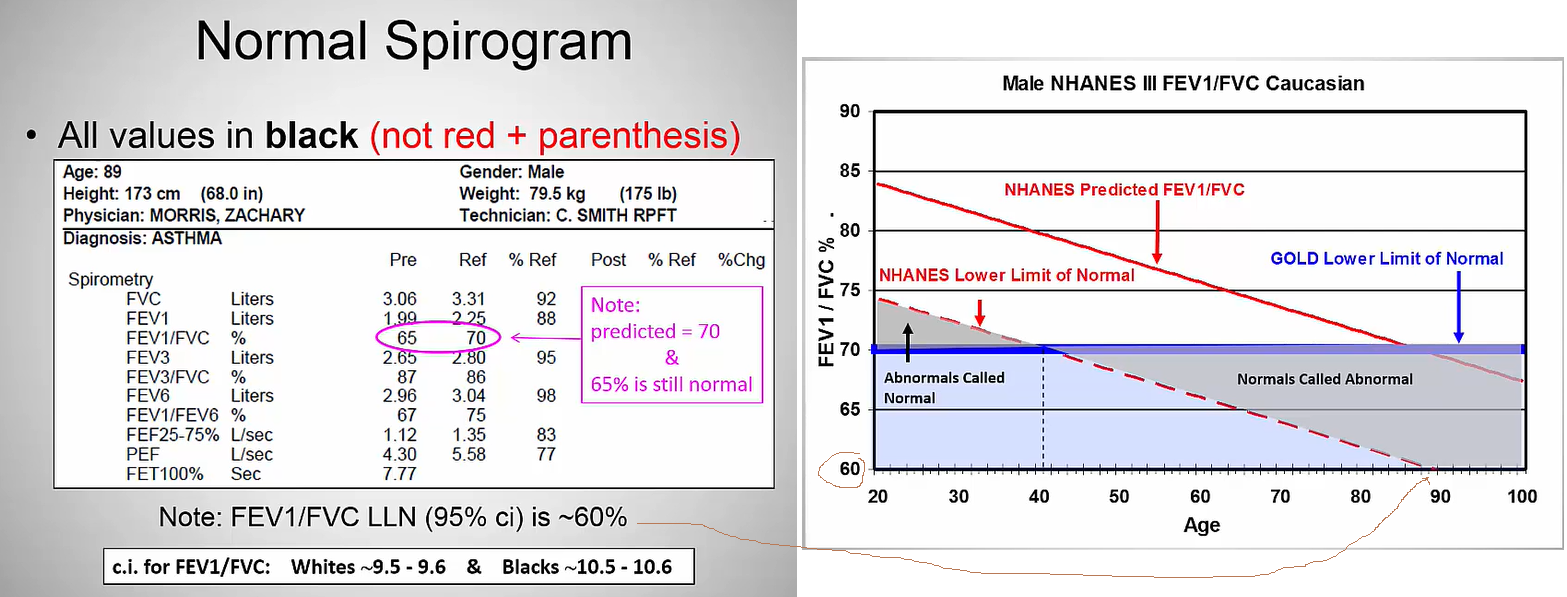
FEV1/FVC should be >
80% in ages up to 18?
CBABE: Cystic fibrosis, Bronchiectasis, Asthma, Bronchitis, Emphysema --> can't get air out of lungs [inc'd TLC, inc'd RV] due to increased airways resistance --> chronic air trapping. On Physical exam: expiratory wheezing
All others are restrictive dzs: PTX, pneumonia, ARDS, IPF, ILD, obesity, kyphoscoliosis --> can't get air into the lungs [dec'd TLC]. On physical exam: can hear velcro-like sounds
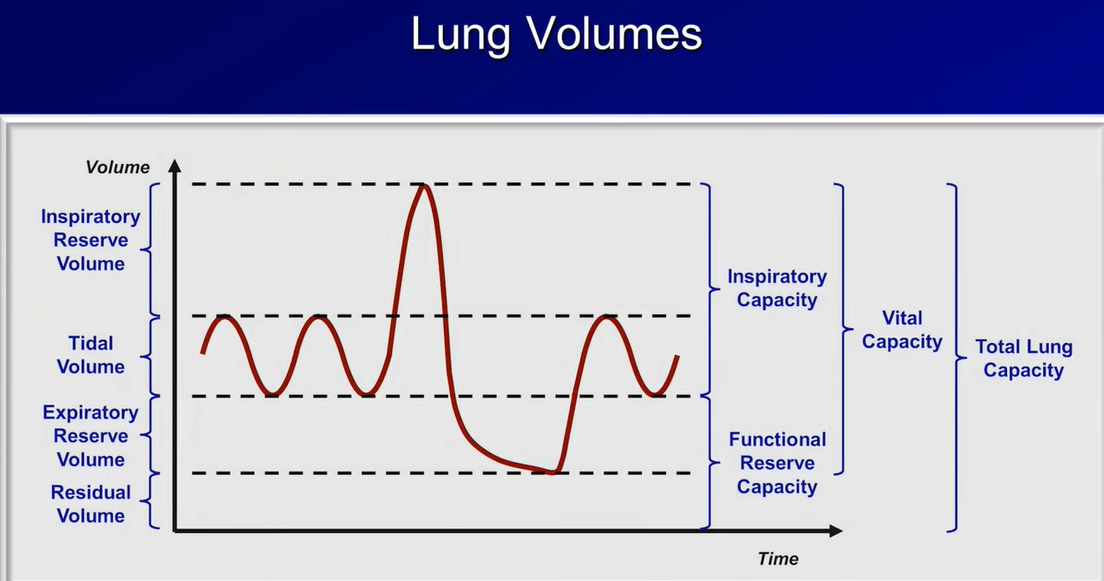
In the FVC maneuver, the pt will inhale as much as he can to "inspiratory capacity" & then forcefully exhale to RV.
In the Volume-Time graph: a slow rise to plateau suggests obstruction.
RV should make up ~ 20% of your TLC. Or, RV/TLC ~ 20%. Abnormal is RV/TLC > 30-35%.
If you have increased TLC and increased RV but normal RV/TLC (< 35%) since RV increases proportionately with TLC --> think chronic hyperinflation --> think COPD
If you have normal TLC (ie, between 80 - 120% pred), but increased RV/TLC (> 35%) --> think acute air trapping --> think Asthma or status asthmaticus
In COPD, chronic air trapping leads to chronic hyperinflation, which causes the TLC to increase. The RV also increases in proportion to the increase in TLC . This causes the RV to TLC ratio to remain approximately normal at ~ 30%.
However, with acute asthma, there is no CHRONIC air trapping; thus, TLC remains normal, but RV increases due to the acute obstructive exacerbation event. his causes RV to increase out of proportion to the normal TLC --> RV/TLC that is elevated.
Videos:
Respiratory Therapy - Pulmonary Function Test Series (1/4) - FVC, FEV1, and the key...FEV1%
ERV: if high in the face of restrictive lung dz pattern, suggests that the restriction is NOT related to obesity.
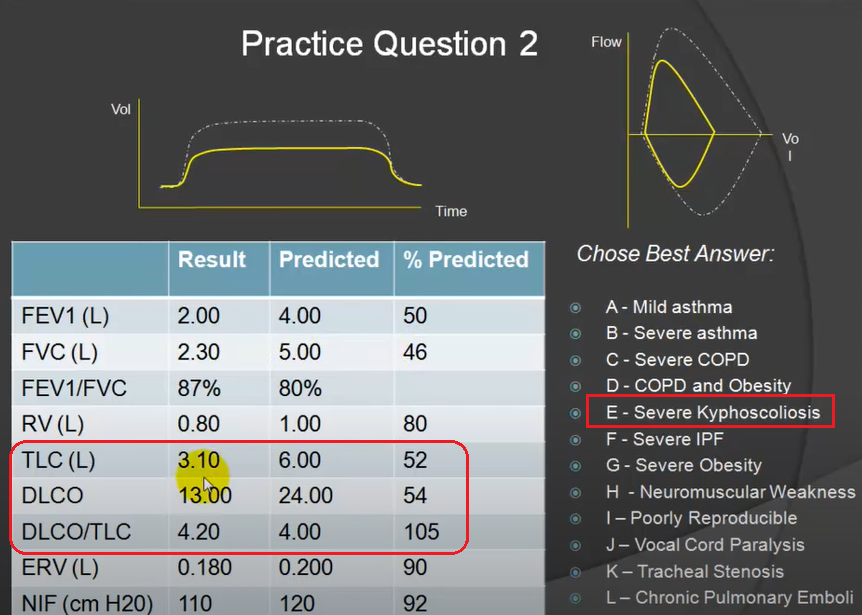
DLCO/TLC: in the face of restrictive disease (decreased TLC) that proportionately decreases the DLCO: if DLCO/TLC is normal, suggests squeezing healthy lungs into small quarters, eg, with severe kyphoscoliosis
Videos:
Obstruction with hyperinflation ATS
Mixed obstructive/restrictive ATS
post-bronchodilator response ATS
Fixed upper airway stenosis ATS
DLCO
Normal = 80 -120%
must be corrected for hemoglobin value
decreased by BOTH obstructive & restrictive dzs! So, DLCO doesn't, by itself, help you distinguish between obstructive vs restrictive process.
problems with pulmonary blood flow, such as pulm HTN can also affect DLCO.
Video:
Respiratory Therapy - Pulmonary Function Testing - Part 3/4 - Diffusion Capacity
Restrictive Pathology
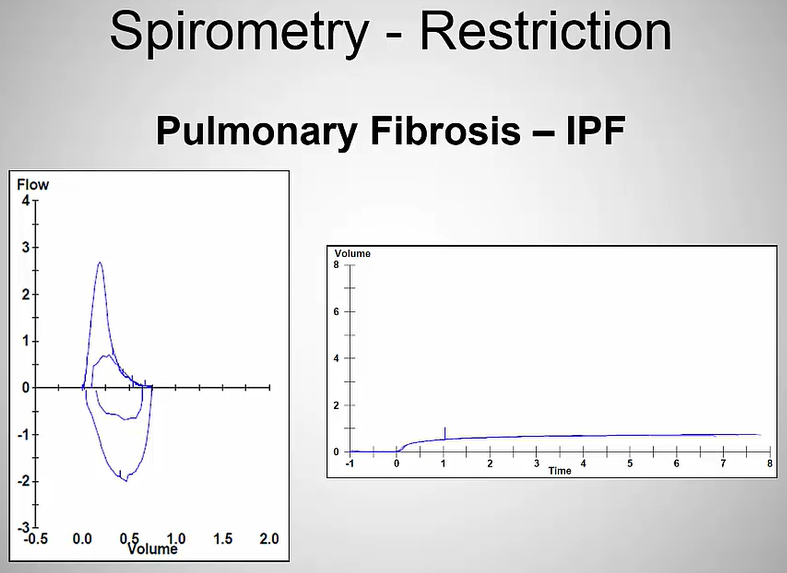 Note the low expiratory volumes in the Volume-time graph
Note the low expiratory volumes in the Volume-time graph
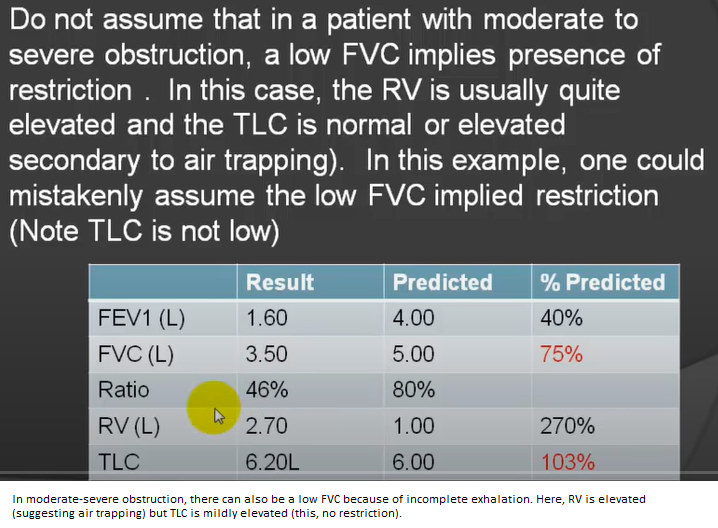
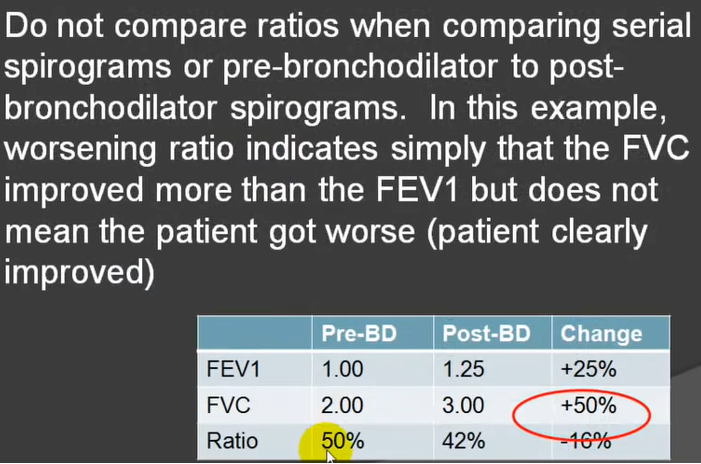
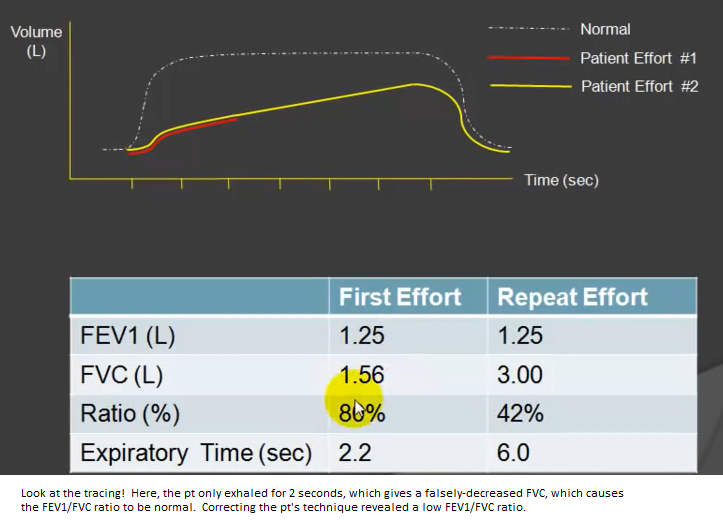
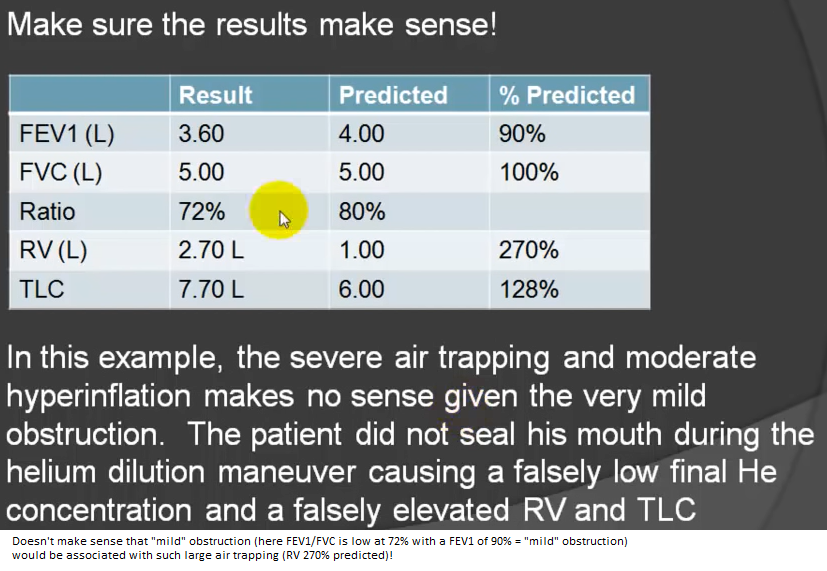
Pitfalls