Arterial oxygen saturation is the percentage of hemoglobin binding sites occupied by O2, which, in turn, is a function of the arterial oxygen pressure/tension (PaO2), as defined by the hemoglobin-oxygen dissociation curve.
An alternative approach used in clinical practice is the assessment of peripheral oxygen saturation (SpO2) using pulse oximetry. This serves as a rapid, non-invasive method of estimating oxygenation and has other benefits such as being continuous, so is able to highlight sudden changes in a patient’s clinical status.
However, the accuracy of pulse oximetry can be influenced by multiple factors including motion, perfusion and skin pigmentation. It is well known that the two wavelength spectroscopy (660 and 940 nm) technique employed in the pulse oximeter is inaccurate in the presence of certain hemoglobin species, such as methemoglobin & carboxyhemoglobin. Although pulse oximeters are tested extensively in healthy volunteers under controlled settings, the ‘working accuracy’, that is, the real-world accuracy in patients in clinical settings can, at times, be suboptimal. Previous studies have suggested suboptimal accuracy of pulse oximetry in critically unwell intensive care unit patients, and people with conditions such as sickle cell disease during vaso-occlusive crises, which may be relevant given the high incidence of thrombotic disease in people with COVID-19. The accuracy of pulse oximetry in these patients has also been identified as a potential contributing factor to apparent ‘silent hypoxia’ seen in COVID-19. Cautions and potential limitations of pulse oximetry in COVID-19 have been highlighted, and one study of 17 patients with COVID-19 on intensive care unit (ICU) suggested that SpO2 does not reliably predict SaO2. However, specific data on people with COVID-19 being stepped down to a non-ICU setting, or being transferred to another ICU, are lacking. Furthermore, anecdotal experience from our ICU, and others, suggests that pulse oximetry measurements (SpO2) may not accurately reflect SaO2 in patients with severe COVID-19, potentially bringing into question the appropriateness of the NHS guidance referenced above in our setting.
However, it is probable that in certain situations, pulse oximetry-derived SpO2 will not be deemed sufficient to guide clinical management and that SaO2 assessment may be required.
The systems described above estimate the oxygen saturation by shining two wavelengths of light (660 and 940 nm) from light-emitting diodes through a cutaneous vascular bed to a sensor on the other side of the tissue. Whereas in the hospital setting, the fingers and earlobes are the typical monitoring sites, the pocket oximeters and phone-based systems utilize only the fingers. Because hemoglobin absorbs these wavelengths of light to different degrees depending on the extent to which binding sites are occupied, varying amounts of light make it through the cutaneous bed to a detector located opposite the emitter. After subtracting out the constant absorption by hemoglobin in capillary and venous blood as well as that by nonvascular structures, the device then uses an internal algorithm to convert the absorbance pattern into an estimate of the arterial oxygen saturation. Pulsatile arterial flow is critical to this measurement, as it is the only means by which the arterial signal can be identified and separated from the other factors that absorb the two wavelengths of light.
Sources:
Noninvasive Ventilatory Support of COVID-19 Patients Outside the ICU
Annals of the American Thoracic Society
TAKE-HOME MESSAGE
The authors of this prospective, single-day, observational study describe the use of noninvasive ventilation in patients with COVID-19 admitted to non-ICU hospital beds. Overall, 909 patients were receiving noninvasive ventilation among a total of 8753 observed patients. Of these, 85% received CPAP, with a helmet interface being the most common mode of delivery. Noninvasive ventilation failed in 300 (37.6%) of these patients, and overall mortality was 25%. Higher C-reactive protein, lower PaO2/FiO2, and platelet counts were each independently associated with higher risk of noninvasive ventilatory failure.
Results from this observational study, although limited in methodology, demonstrate the use of noninvasive ventilatory support in patients with COVID-19 admitted outside of the ICU setting, and suggest that C-reactive protein, PaO2/FiO2, and platelet count may be helpful in identifying patients at higher risk of needing additional support.
Hypoxemia
The most common causes of refractory hypoxemia are divided into cardiac & pulmonary. The most common pulmonary causes are consolidated pneumonitis, atelectasis, neoplasm, or the ARDS/acute lung injury.
Methods of improving oxygenation include prone positioning, which increases the homogeneity of the intrapulmonary process & improves ventilation.
Shunt and PEEP
QSP/Qt = (CcO2 – CaO2)/ (CcO2 – CvO2) where Qt is cardiac output
Intrapulmonary shunt is defined as that portion of the cardiac output entering the left side of the heart without undergoing perfect gas exchange with completely functional alveoli. Intrapulmonary shunt can be divided into 3 components.
Since true shunt is not supplemental-oxygen responsive, PEEP therapy may be applied to the diseased lungs to help reduce QSP/QT. Among the physiologic responses seen with PEEP are improved oxygenation, increased functional residual capacity, improved lung compliance and a decrease in shunting.
The decrease in shunting seen with PEEP is most classically attributed to alveolar recruitment or an increase in functional residual capacity secondary to the inflation of previously collapsed alveoli.
Gattinoni has described using computed tomography the regional gas distribution in tissues during the titration of PEEP. These studies have confirmed the classic inflection point in the gas/tissue curve, which is consistent with alveolar recruitment.
The response of PEEP titration varies not only with the type of lung pathology but also with the region of lung studied. More dependent lung regions undergo greater degrees of alveolar recruitment while less dependent lung regions tend to experience greater increases in alveolar volume without recruitment, and regions of lung that are non-responsive to PEEP are equally distributed throughout the lung.
Other methods of improving oxygenation include prone positioning, which increases the homogeneity of the intrapulmonary process and improves ventilation.
Source: https://acutecaretesting.org/en/articles/setting-the-record-straight-on-shunt
For a patient with a good pulse oximetry waveform, pulse oximetry has numerous advantages compared to ABG monitoring:
PaO2, the oxygen tension in arterial blood, is the best way to determine how well the lungs are working. However, oxygen saturation is a better measurement of the systemic oxygen delivery to the tissues (DO2)(7):
DO2 = 13.4(cardiac output)(hemoglobin)(oxygen saturation)
An ABG is painful for the wrist and the wallet. The total cost of drawing and analyzing an ABG is nearly $200 (1). In contrast, pulse oximetry is noninvasive, painless, and free (2).
If you’re using the ABG as a therapeutic monitoring tool, then one ABG is rarely enough. The first ABG will often reveal some abnormality, leading to a minor change in the ventilator and repeat ABG. But the second ABG isn’t quite right, so you tweak the ventilator some more and get another ABG. Before you know it, you’ve ordered a cascade of ABGs and minor ventilator adjustments (with no real benefit to the patient).
Occasionally, an arterial catheter might even be placed for the purpose of measuring frequent ABGs. This is generally a terrible idea. The availability of an easy source of arterial blood encourages frequent ABGs and other labs as well. For example, one study found that the presence of an arterial catheter correlated with a four-fold greater volume of phlebotomy (Tarpey 1990).
Infrequently, ABGs will actually represent a venous or mixed sample. The oxygen extraction of the hand isn’t very high, so the level of oxygen in these venous samples may be only slightly lower than arterial blood. Thus, it may not be obvious that the sample was venous.
Many hospitals utilize point-of-care ABG analyzers. These devices typically measure PaO2 & subsequently use this to calculate the O2 saturation (assuming a normal PaO2 vs. oxygen saturation curve). For pts with abnormal hemoglobin dissociation curves, this calculated saturation will be wrong.
The Haldane effect is a physicochemical phenomenon which describes the increased capacity of blood to carry CO2 under conditions of decreased hemoglobin oxygen saturation
Measuring an ABG may delay interventions, such as ICU transfer or intubation. Sometimes it seems like physicians check an ABG when they don’t know what to do, in order to buy some time to think. At other times, it may seem like the ICU team requests an ABG to delay accepting a patient. Occasionally, physicians may feel obligated to check an ABG before calling for help, to exercise due diligence. Regardless, the practice of delaying treatment to obtain an ABG is usually unnecessary, particularly when oxygenation is concerned (3).
We are constantly exposed to oxygen saturation values, leading to the development of a good sense about what they mean. Meanwhile, we are exposed to PaO2 values far less often, so we may struggle to interpret them.
The most common error is panicking about a low PaO2 value. PaO2 values are always much lower than oxygen saturation values. This is simply a reflection of the oxygen saturation curve (figure above). For example, a saturation of 88% correlates to a PaO2 of ~55mm. We’re generally comfortable with a saturation of 88%, but a PaO2 of 55mm may cause concern. The lower number is scarier.
This cognitive bias is often seen when ABGs are obtained in patients on mechanical ventilation. For a patient with mild hypoxemia, the PaO2 value will often be surprisingly low. This may lead to unnecessary increases in FiO2 and PEEP, delaying extubation.
The A-a gradient is the difference in oxygen tension between arterial blood and alveolar gas. Medical school courses love this. However, trying to use the ABG to diagnose the etiology of respiratory failure works poorly in real life:
I sometimes see practitioners measure the A-a gradient of a critically ill patient who is requiring moderate to high levels of supplemental oxygen (e.g. >3 liters/min). Measuring this is pointless, because such patients will invariably have an elevated A-a gradient (if the patient had a normal A-a gradient, then they would require at most a low amount of supplemental oxygen)(4).
We’ve all been called to evaluate a patient for low oxygen saturation. Often, the saturation will bounce back rapidly on its own. Thus, we are constantly paying attention to oxygenation trends and averaging the oxygen saturation over time. Nurses are often keenly aware of this (“yeah, he desats whenever he starts coughing, don’t worry he’ll be fine in a minute”).
If we obtain an ABG, this sort of trending and averaging is impossible. We have access to only one point in time. It is impossible to know whether the oxygen saturation was transiently low, or if it was continuously low. The usual assumption is that the ABG reflects the patient’s ongoing condition (for example, if the patient was hypoxemic 15 minutes ago, then they must still be hypoxemic now). This assumption is frequently wrong.
Let’s imagine that we obtain 2 ABGs to determine if there has been any change in oxygenation after initiating BiPAP. After starting BiPAP, the PaO2 decreases from 56 mm down to 49 mm. The oxygenation is worsening, so this indicates that we must intubate the patient.
No, it doesn’t. Please step away from the laryngoscope. Mallat 2015 compared back-to-back ABGs drawn via arterial catheters in 129 ICU pts to determine the repeatability of this test. There are large differences between these nearly simultaneous PaO2 values. The 95% confidence interval in comparing two PaO2 values was +/- 9mm:
This is consistent with previous studies (5). Therefore, PaO2 differences in sequential ABGs will often reflect merely random variation. To be >95% confident that a difference doesn’t represent random noise, it should be >9mm. However, to be >95% confident that the a clinically significant change occurred (let’s say, >10mm change), the measured difference must be even higher, perhaps >19mm.
Changes in pulse oximetry are more likely to be meaningful, because the provider will typically look at numerous values over time. For example, if a pt had been consistently saturating in the high 90’s and is now consistently saturating in the 80s, we can be fairly confident that there has been a change (rather than representing two data points, this represents dozens of data points).
There are some situations when it may be helpful to use an ABG to investigate oxygenation.
The most common situation where ABG is needed to test oxygenation is when pulse oximetry cannot provide a reliable waveform. For example, some pts have non-pulsatile blood flow from a ventricular assist device (VAD) or ECMO. Poor perfusion may lead to an erratic waveform.
Methemoglobinemia will artificially lower the pt's measured O2 saturation, usually producing saturations between 85-90%. This will typically cause providers to give more oxygen, which doesn’t improve the measured oxygen saturation. In this context, mismatch between the low saturation versus the PaO2 (which will often be elevated) suggests a diagnosis of methemoglobinemia.
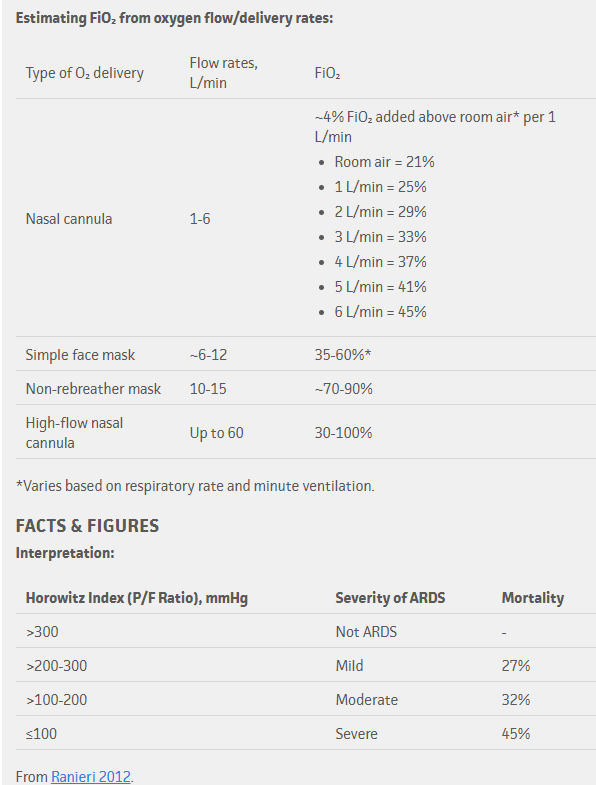
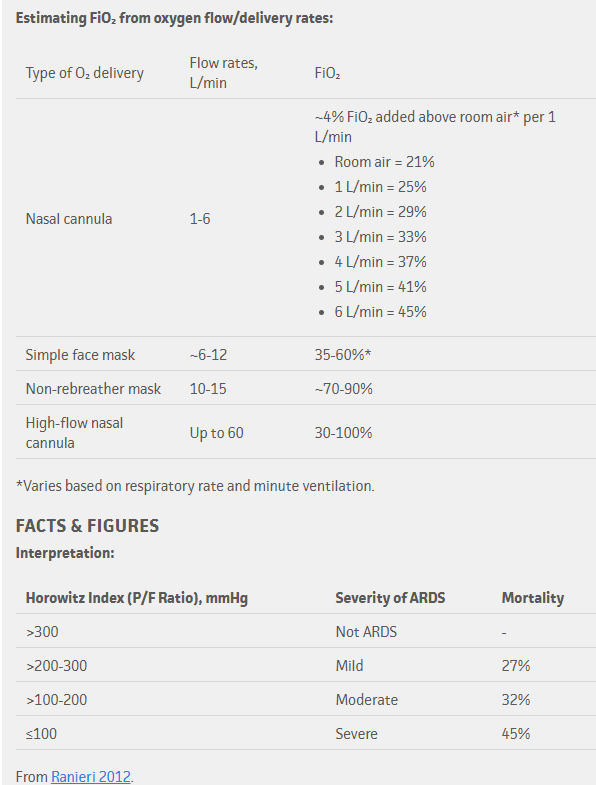
The PaO2/FiO2 ratio is often used as an index of severity of hypoxemia among pts who are intubated. Most evidence on proning in ARDS was performed using the PaO2/FiO2 ratio, including cutoffs determining which pts benefit. Thus, knowing the PaO2/FiO2 ratio may be helpful if you are contemplating whether to prone a pt.
More information isn’t always better. One example of this can be borrowed from a post by Rory Speigel about the use of brain natriuretic peptide (BNP) for diagnosing heart failure. BNP has very good test characteristics for diagnosing heart failure. However, in clinical practice it doesn’t seem to help much. Why not?
The answer is that clinicians are very good at diagnosing heart failure without BNP. Thus, it’s unlikely that the BNP will improve our performance much. BNP could also point us in the wrong direction. It adds more information, but not necessarily superior information to what we already have.
Adding a PaO2 to an oxygen saturation is similar. Oxygen saturation alone is an excellent measurement of the pt's oxygenation. For most pts, it is unclear what PaO2 adds above & beyond the oxygen saturation. The added information may be more likely to mislead than to inform.
For patients with an adequate oximetry waveform, pulse oximetry is usually superior to ABG for measuring oxygenation. The top 10 reasons for this are:
Source: https://emcrit.org/pulmcrit/pulse-oximetry/