PNEUMONIA
xxxxx
Pneumonia
Essentials of Diagnosis
Hospital-acquired pneumonia (HAP) is diagnosed in pt with clinical features & imaging consistent with pneumonia, occurring > 48 hours after admission to the hospital, & excluding any infections present at the time of admission
Ventilator-associated pneumonia (VAP) requires clinical features concerning for new pneumonia with positive respiratory samples developing > 48 hours following endotracheal intubation & mechanical ventilation
General Considerations
Most common organisms in HAP
- Staphylococcus aureus (both methicillin-sensitive S aureus & methicillin-resistant S aureus)
- Pseudomonas aeruginosa
- Gram-negative rods, including non–extended-spectrum β-lactamase (non-ESBL) producing and ESBL-producing (Enterobacter species, Klebsiella pneumoniae, and Escherichia coli)
Organisms seen in VAP
- Acinetobacter species
- Stenotrophomonas maltophilia
Anaerobic organisms may also cause pneumonia in the hospitalized patient
- Bacteroides
- Anaerobic streptococci
- Fusobacterium
Uncommon causes of nosocomial pneumonias
- Mycobacteria
- Fungi
- Chlamydiae
- Viruses
- Rickettsiae
- Protozoal organisms
Symptoms and Signs
Nonspecific
However, 2 or more clinical findings (fever, leukocytosis, purulent sputum, worsening respiratory status) along with one or more new or progressive pulmonary opacities on chest imaging are characteristic features
Differential Diagnosis
- Heart failure
- Atelectasis
- Aspiration
- Acute respiratory distress syndrome (ARDS)
- Pulmonary thromboembolism
- Pulmonary hemorrhage
- Medication reactions
Laboratory Tests
Blood cultures identify the pathogen in up to 15–20% of cases
Complete blood count and chemistry tests
- Not helpful in identifying the etiologic agent
- However, can assist in determining illness severity and complications
Gram stains and other examinations of respiratory secretions & cultures of respiratory secretions are controversial but may be useful in guiding antibiotic therapy
Serum procalcitonin levels are not sufficiently sensitive to rule out HAP or VAP but may allow discontinuation of antibiotic therapy
Imaging Studies
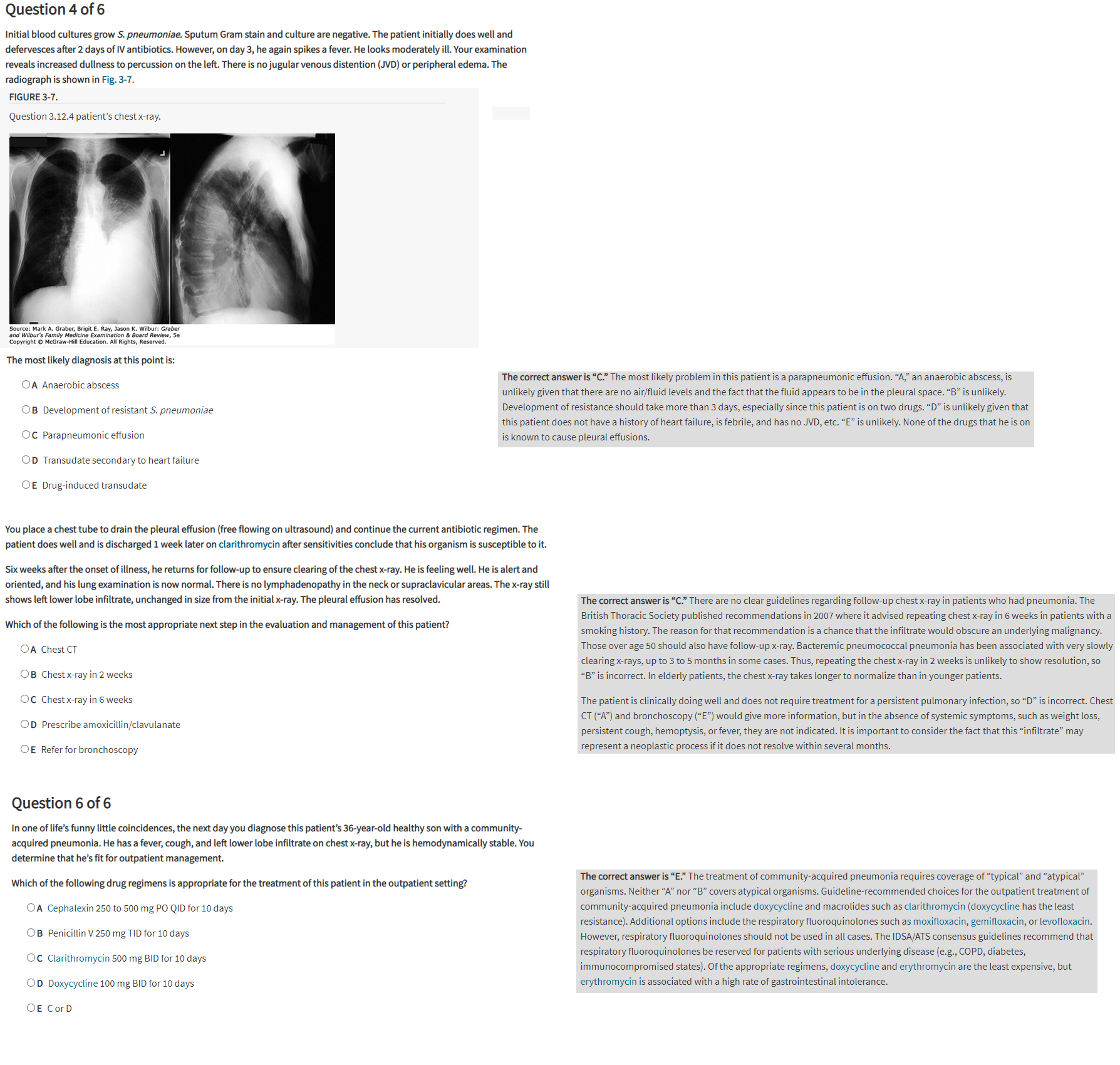
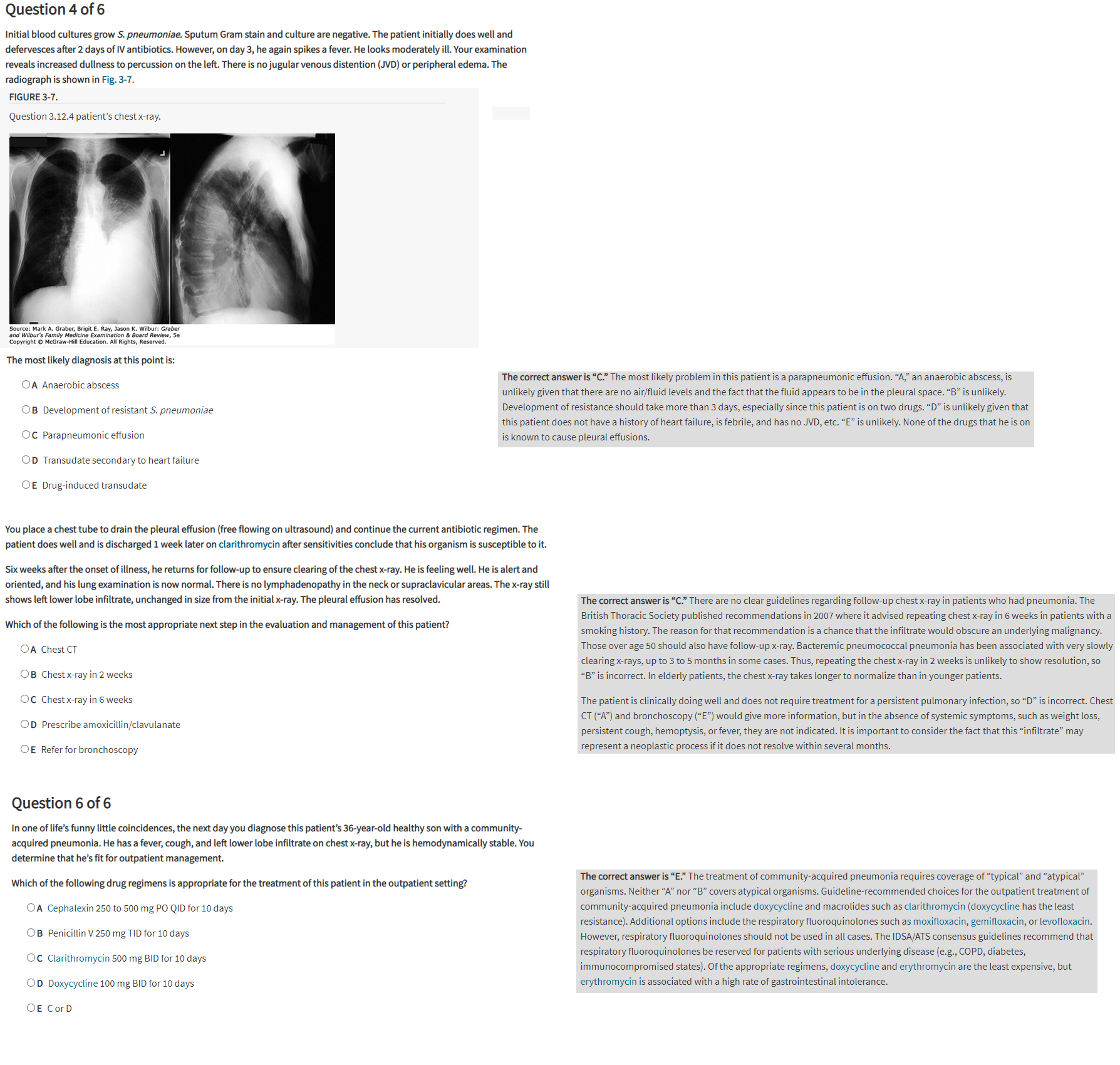
Radiographic findings
- Nonspecific
- Range from patchy opacities to lobar consolidation to diffuse alveolar or interstitial opacities
Diagnostic Procedures
When HAP is suspected in a pt who subsequently requires mechanical ventilation, secretions may be obtained by
- Spontaneous expectoration
- Sputum induction
- Nasotracheal suctioning
- Endotracheal aspiration (qualitative or semiquantitative samples)
- More likely to return nonpathogenic organisms
- Thus, associated with higher antibiotic exposure (without improvement in mortality)
- Bronchoscopic sampling of the lower airways secretions (quantitative samples): increases cost & patient risk
Invasive qualitative sampling is universally recommended when
- The patient is not improving with initial therapy directed at the expected or isolated pathogens
- An opportunistic pathogen is suspected in an immunocompromised person
Medications
- See Tables 9–11 and 30–5
- Treatment is usually empiric and should be started as soon as the diagnosis is suspected
- No consensus regimens exist, but guidelines separate patients by disease severity
- Therapy for gram-negative bacterial pneumonia is typically continued for at least 8 days
- Data from a large trial assessing treatment outcomes in ventilator-associated pneumonia suggest that 8 days of antibiotics is as good as 15 days