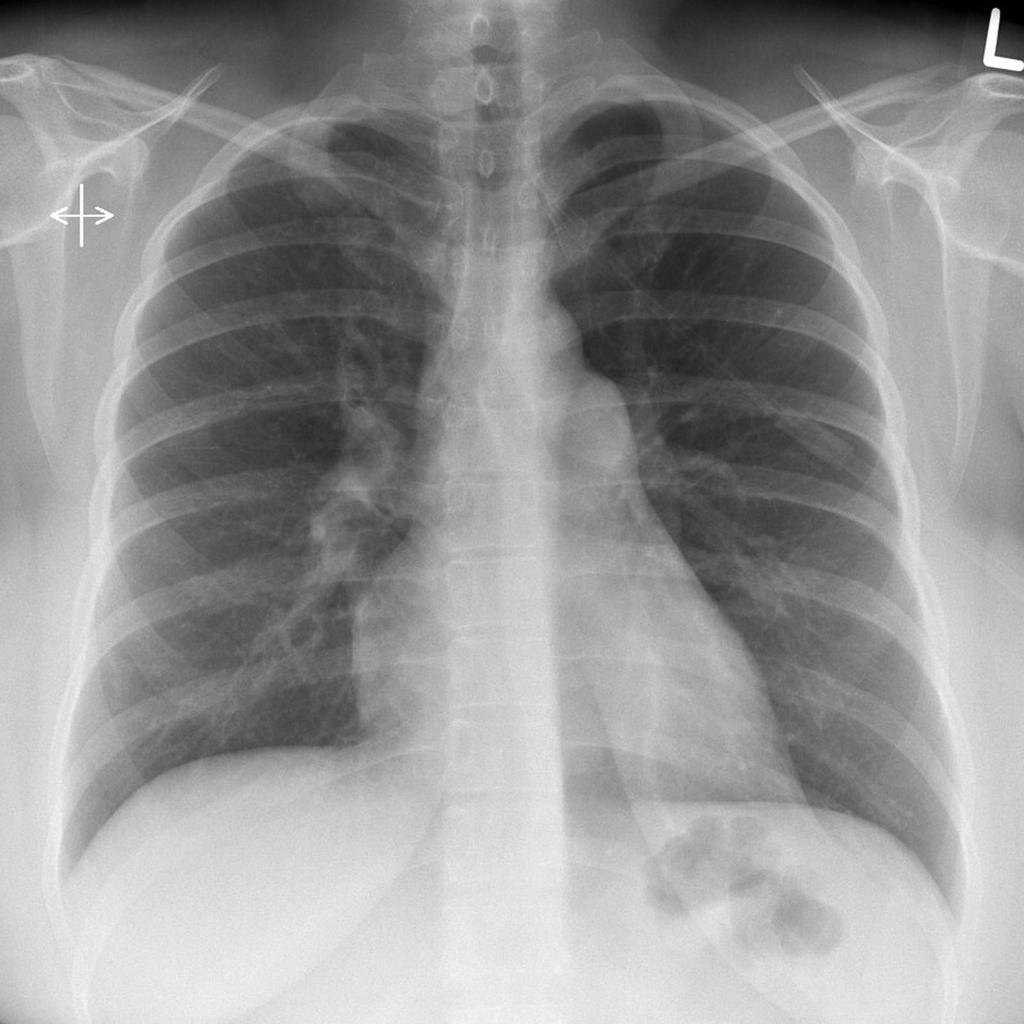
A 37-year-old woman is referred to the pulmonologist’s office from her PCP for worsening shortness of breath. She reports that she has had increasing dyspnea on exertion and fatigue for the past 3 years, but it has gotten much worse in the last 2 months. She used to walk around the neighborhood with her friends but now gets short of breath with occasional chest pain just walking around the house. Her past medical history is otherwise completely negative. On physical exam, she has a JVP of 13 cm H2O, a loud P2, an S3, a right-sided heave, a liver palpable 3 cm below the costal margin, and bilateral leg edema. She is sent for a trans-thoracic echocardiogram which estimates a high pulmonary artery systolic pressure and shows right ventricular hypertrophy and right heart failure. The diagnosis is confirmed with a right heart catheterization and she is started on epoprostenol.
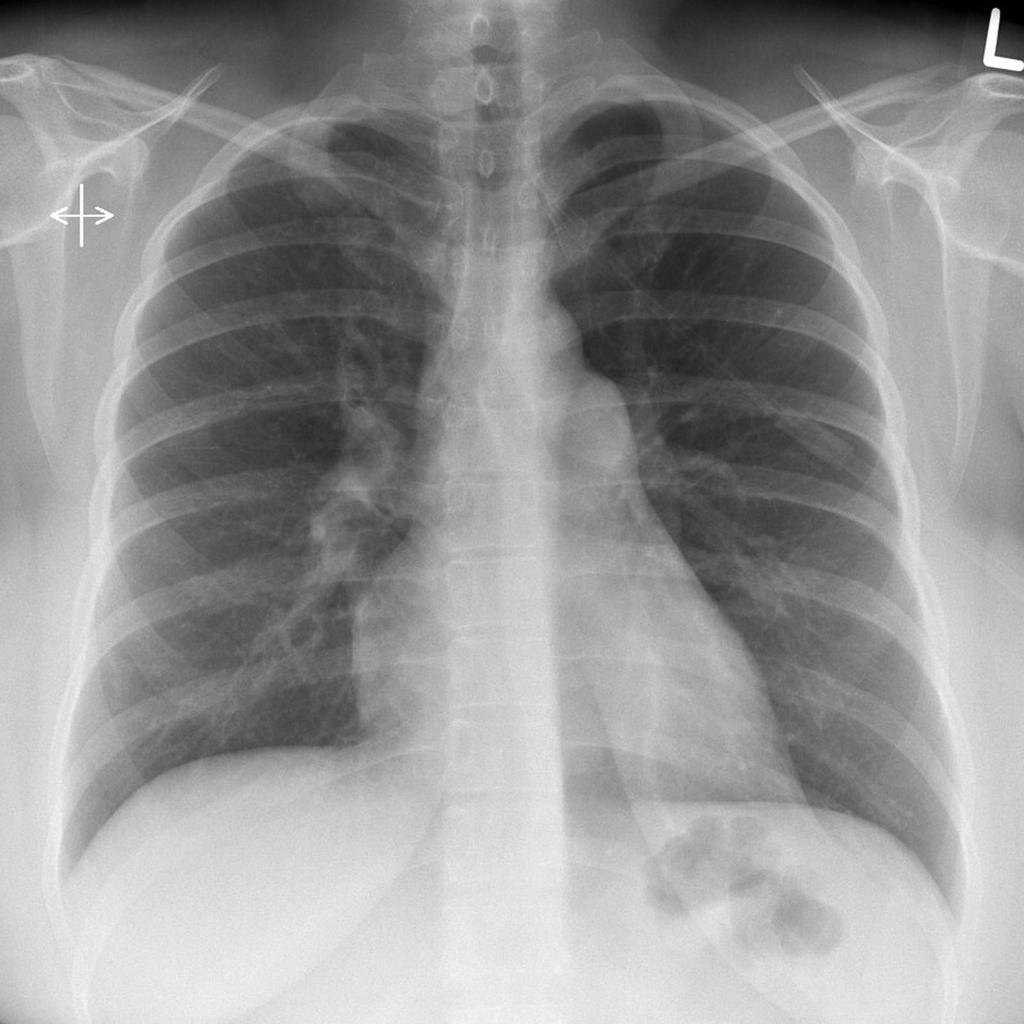
 CT Angiogram, coronal of pulm HTN
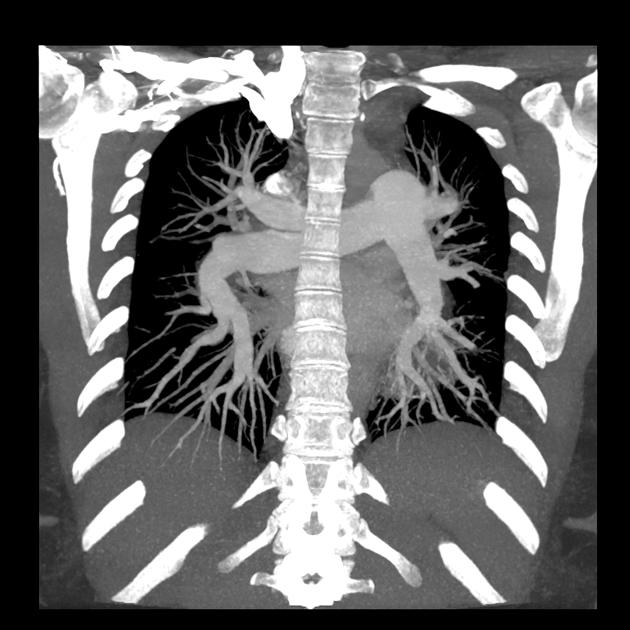
CT Angiogram, coronal of pulm HTN  CTA, axial view
CTA, axial view
| Etiologies of Pulmonary Hypertension | |
|
Primary Etiologies |
|
| Etiology | Key Points |
| Idiopathic pulmonary arterial hypertension (IPAH) |
|
| Hereditary pulmonary arterial hypertension (HPAH) |
|
|
Secondary Etiologies |
|
| Etiology (secondary to) | Key Points |
| Autoimmune disease |
|
| Drugs |
|
| Infection |
|
| Left-to-right shunt |
|
| Left heart disease |
|
| Lung disease/hypoxia |
|
| Thromboembolic disease |
|
| Unclear/miscellaneous |
|
|
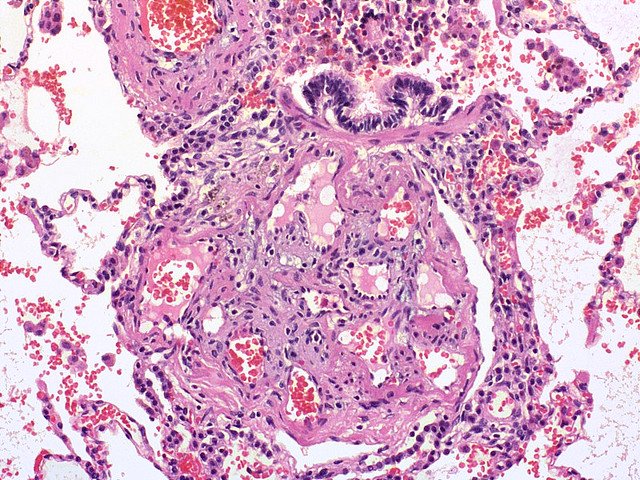
Presentation |
|
Source:
https://step1.medbullets.com/respiratory/117016/pulmonary-hypertension