2020 Asthma Guidelines Dr. Michael Wechsler
Source: Asthma and COPD: Stable Disease - Diagnosis and Management -- Dr Eric Strong
REACTIVE AIRWAYS DISEASE
Sometimes the terms "reactive airway disease" and "asthma" are used interchangeably, but they are not the same thing. Often, the term "reactive airway disease" is used when asthma is suspected, but not yet confirmed.
Reactive airway disease in children is a general term that doesn't indicate a specific diagnosis. It might be used to describe a history of coughing, wheezing or shortness of breath triggered by infection. These signs and symptoms might or might not be caused by asthma.
Describing a condition as reactive airway disease in part reflects the difficulty in establishing a diagnosis of asthma in some situations — such as during early childhood. Although it's possible for infants and toddlers to have asthma, tests to diagnose asthma generally aren't accurate before age 5.
ASTHMA
Asthma
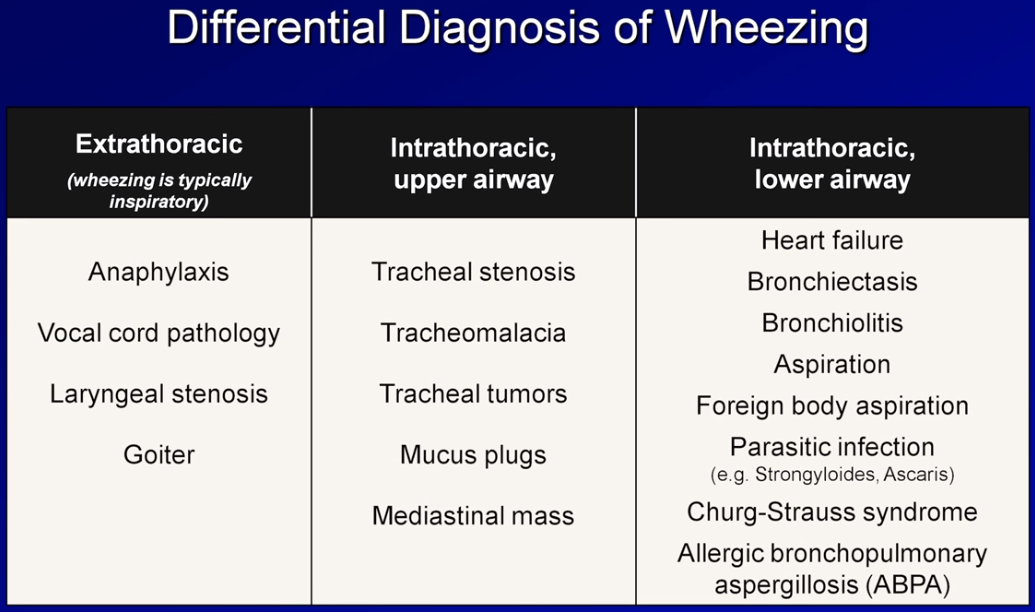
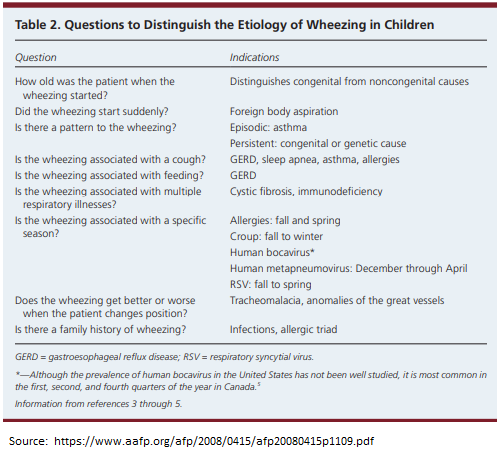
The most common causes of wheezing in children include asthma, allergies, infections, GERD, obstructive sleep apnea. Less common causes include congenital abnormalities, foreign body aspiration, & cystic fibrosis.
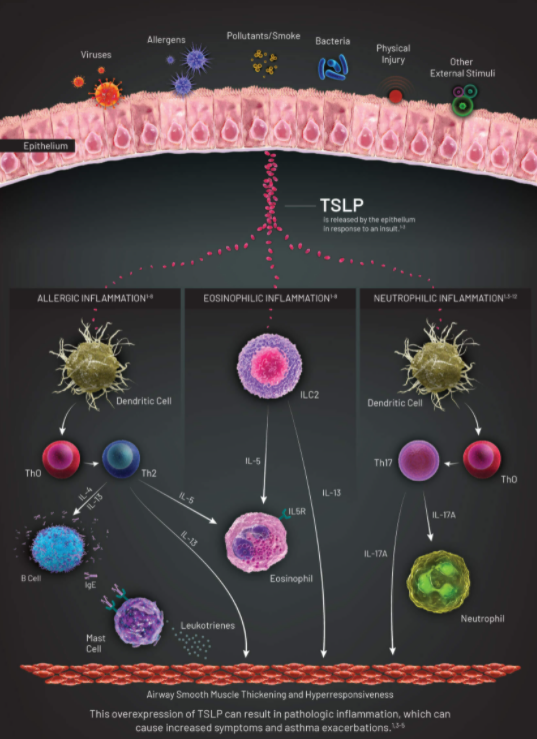
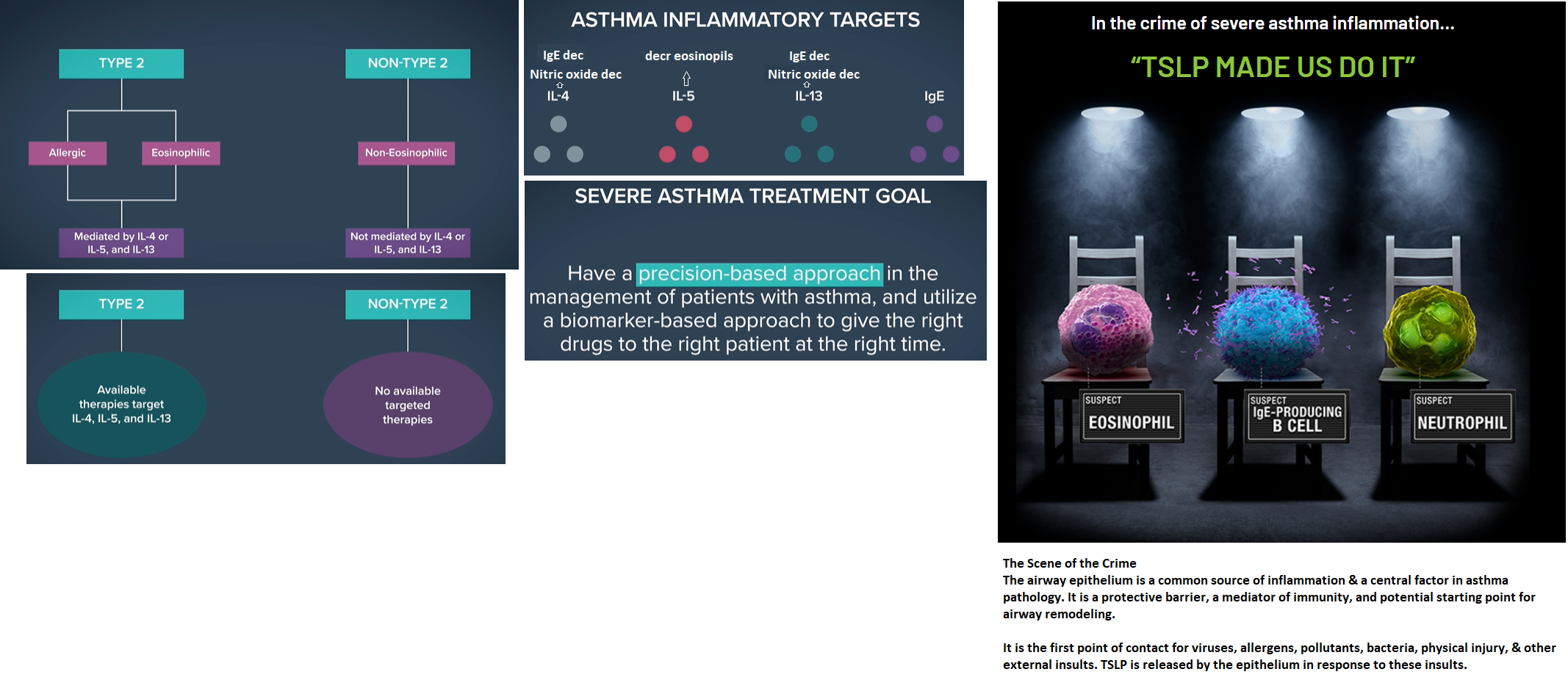
Asthma is classified as either “allergic asthma” or “non-allergic asthma.” While non-allergic asthma can occur independently of any allergens, allergic asthma is triggered by certain substances, as mentioned above. Common irritants also will worsen allergic asthma, such as smoking (cigarettes, marijuana or e-cigarettes), air pollution, air fresheners, cleaning agents and artificial fragrances.
Children who have seasonal allergies also may experience an influx of asthmatic symptoms during certain months. For instance, in spring there’s more pollen in the air, which can aggravate hay fever, eczema and, of course, asthma. If your child is experiencing coughing, wheezing and/or shortness of breath in conjunction with hay fever or skin irritation, then they likely have allergic asthma.
The main symptom of asthma is a persistent cough, which often occurs at night. If the condition worsens, symptoms may include wheezing, tightness in the chest or even shortness of breath. In children with non-allergic asthma, exercise, colds & sinus infections also can aggravate these symptoms. A family history of asthma may predict your child’s likelihood of developing this condition.
Caused by an overactive immune system, allergies can affect children of all ages, just like asthma. During allergic reactions to substances like pollen, a child often will develop nasal congestion, runny nose and/or itchy eyes. These allergy-provoking substances—referred to as allergens—often include things such as dander, grass, pollen, mold or dust mites. Similar to asthma, a family history of allergies makes it more likely for your child to experience allergic reactions.
Asthma Dx
Source:
PFT for Fellows (Spiro) 08192016
COPD Inpatient
CBC, CXR, influenza nasal swab (seasonal), ECG
?: procalcitonin
Source: http://www.med.umich.edu/1info/FHP/practiceguides/InptCOPD/COPD.final.pdf
COPD Outpt Case
A 62-year-old man presents to your office for an acute visit because of coughing and shortness of breath. He is well known to you because of multiple office visits in the past few years for similar reasons. He has a chronic “smoker’s cough” but reports that in the past 2 days his cough has increased, his sputum has changed from white to green in color, and he has had to increase the frequency with which he uses his albuterol inhaler. He denies having a fever, chest pain, peripheral edema, or other symptoms. His medical history is significant for hypertension, peripheral vascular disease, and two hospitalizations for pneumonia in the past 5 years. He has a 60 pack-year history of smoking and continues to smoke two packs of cigarettes a day.
On examination, he is in moderate respiratory distress. His temperature is 98.4 °F, his blood pressure is 152/95 mm Hg, his pulse is 98 beats/min, his respiratory rate is 24 breaths/min, and he has an oxygen saturation of 94% on room air. His lung examination is significant for diffuse expiratory wheezing and a prolonged expiratory phase of respiration. There are no signs of cyanosis. The remainder of his examination is normal. A chest x-ray done in your office shows an increased anteroposterior (AP) diameter and flattened diaphragm, but otherwise he has clear lung fields.
Questions
What is the most likely cause of this patient’s dyspnea?
What acute treatment(s) are most appropriate at this time?
What interventions would be most helpful to reduce the risk of future episodes similar to this one?
Answers to Case 2: Dyspnea (Chronic Obstructive Pulmonary Disease)
Summary: A 62-year-old man presents with
A long history of smoking
Dyspnea, coughing, and wheezing
Increased sputum production and a change in sputum character
Most likely cause of dyspnea: Acute exacerbation of chronic obstructive pulmonary disease (COPD).
Appropriate acute treatments: Antibiotic, bronchodilators, systemic corticosteroids.
Interventions to reduce future exacerbations: Smoking cessation, long-acting bronchodilator, inhaled corticosteroid, influenza, and pneumococcal polysaccharide vaccination.
Analysis
Objectives
Be able to diagnose and determine the stage of COPD in adults. (EPA 1, 3)
Know the management of stable COPD and COPD exacerbations. (EPA 4, 10)
Considerations
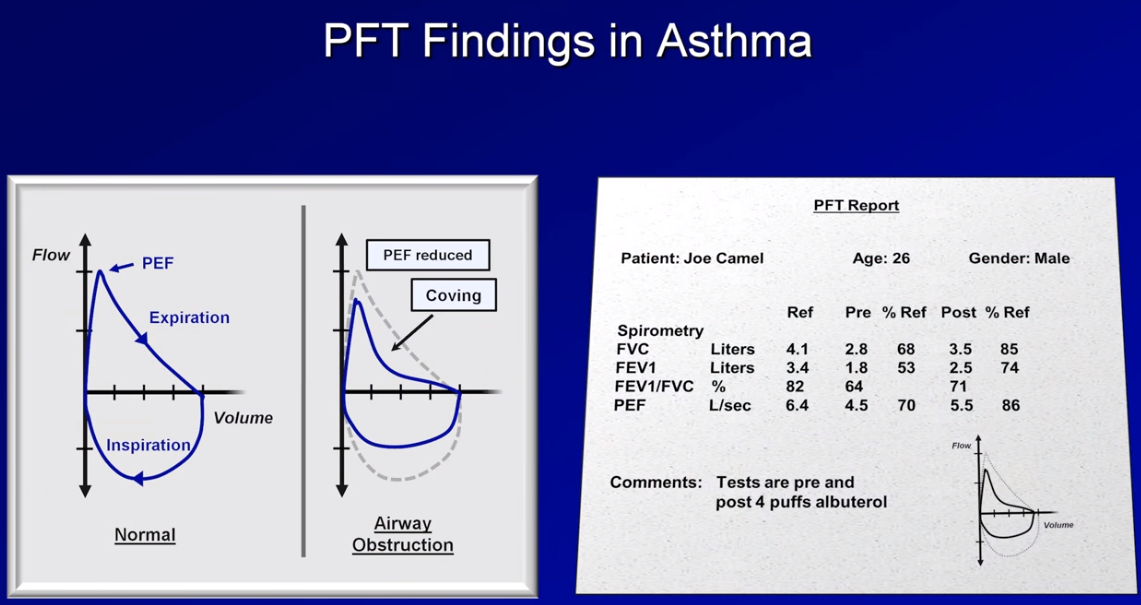
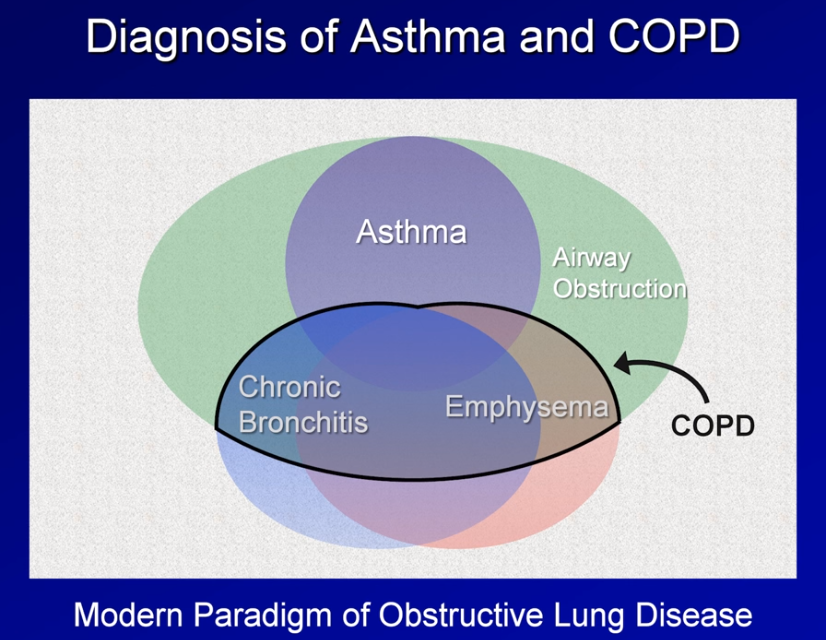
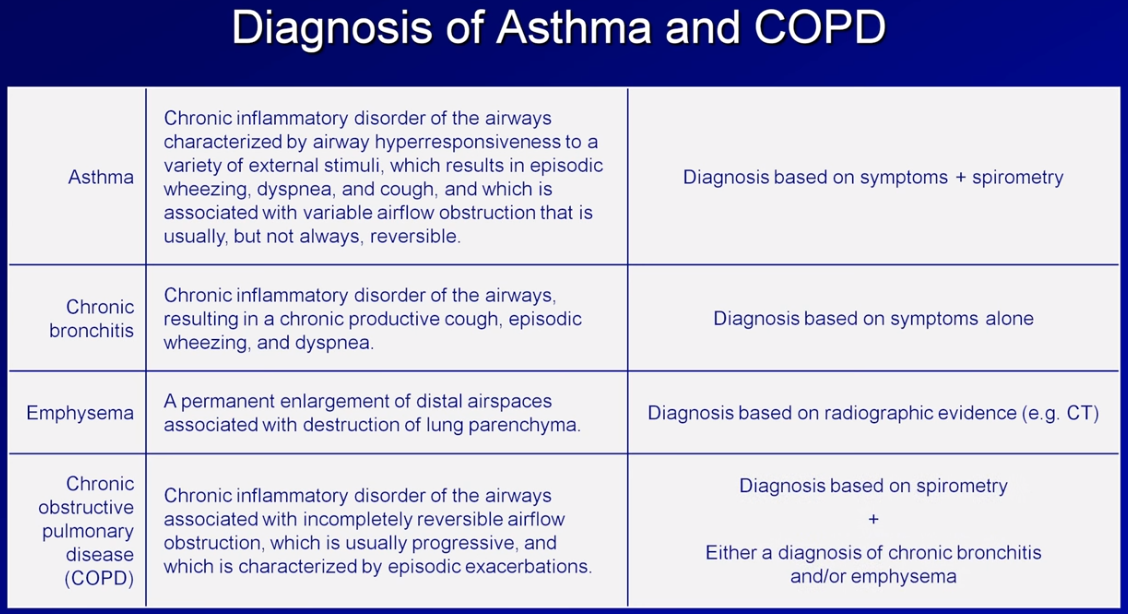
Dyspnea is a common symptom in many diseases. It is important to do an appropriate history, physical examination, and diagnostic testing in order to correctly identify and manage the cause. Two of the most common causes of dyspnea and wheezing in adults are asthma and COPD. There can be substantial overlap between the two diseases, as patients with asthma can develop chronic obstructive disease over time. As in most medical situations, the patient’s history will usually provide the key information for the appropriate diagnosis. Asthma often presents earlier in life, may or may not be associated with cigarette smoking, and is characterized by episodic exacerbations with return to relatively normal baseline lung functioning. COPD, on the other hand, tends to present in midlife or later, is usually the result of a long history of smoking, and is a slowly progressive disorder in which measured pulmonary functioning never returns to normal.
In the setting of an acute exacerbation, the differentiation between an exacerbation of asthma and an exacerbation of COPD is not necessary for determination of the immediate management. The assessment of the patient presenting with dyspnea should always start with the ABCs—Airway, Breathing, and Circulation. Intubation with mechanical ventilation should be performed when the patient is unable to protect his own airway (eg, when the patient has a reduced level of consciousness), when he or she is tiring because of the amount of work required to overcome the airway obstruction, or when adequate oxygenation cannot be maintained.
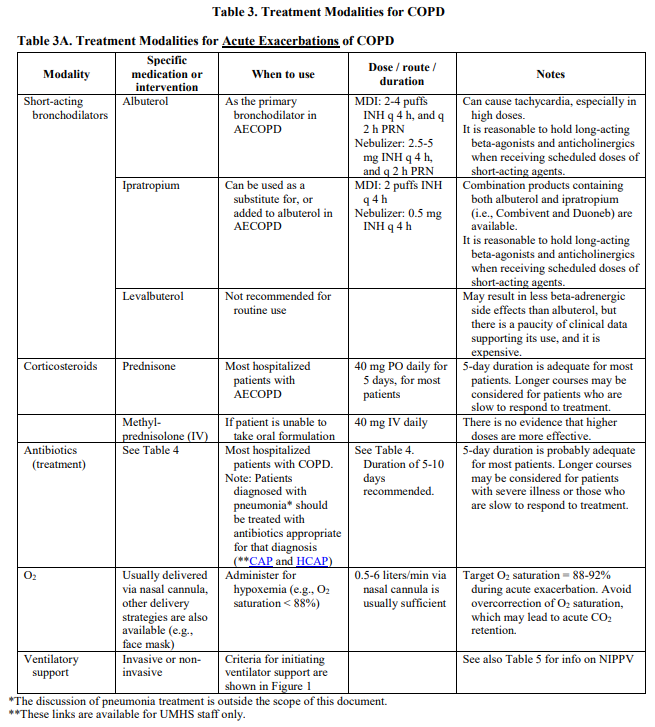
For both asthma and COPD exacerbations, the mainstays of medical therapy are oxygen, bronchodilators, and steroids. All dyspneic patients should have an assessment of their level of oxygenation. Clinical signs of hypoxemia, such as cyanosis of the perioral region or digits, should be noted on examination. Objective levels of oxygenation using pulse oximetry or arterial blood gas measurements should also be performed. Hypoxemia must be addressed by providing supplemental oxygen. Inhaled beta-2 agonists, most commonly albuterol, can rapidly result in bronchodilation and reduction in airway obstruction. The addition of an inhaled anticholinergic agent, such as ipratropium, may work synergistically with the beta-2 agonist. Corticosteroids, given systemically (orally, intramuscularly, or intravenously), act to reduce the airway inflammation that underlies the acute exacerbation. Clinically significant effects of steroids take hours to occur; consequently, steroids should be used with bronchodilators because bronchodilators act rapidly. Steroids used in combination with bronchodilators significantly improve short-term outcomes in the management of acute exacerbations of asthma and COPD.
Definitions
CHRONIC BRONCHITIS: Cough and sputum production on most days for at least 3 months during at least 2 consecutive years.
EMPHYSEMA: Shortness of breath caused by the enlargement of respiratory bronchioles and alveoli caused by destruction of lung tissue.
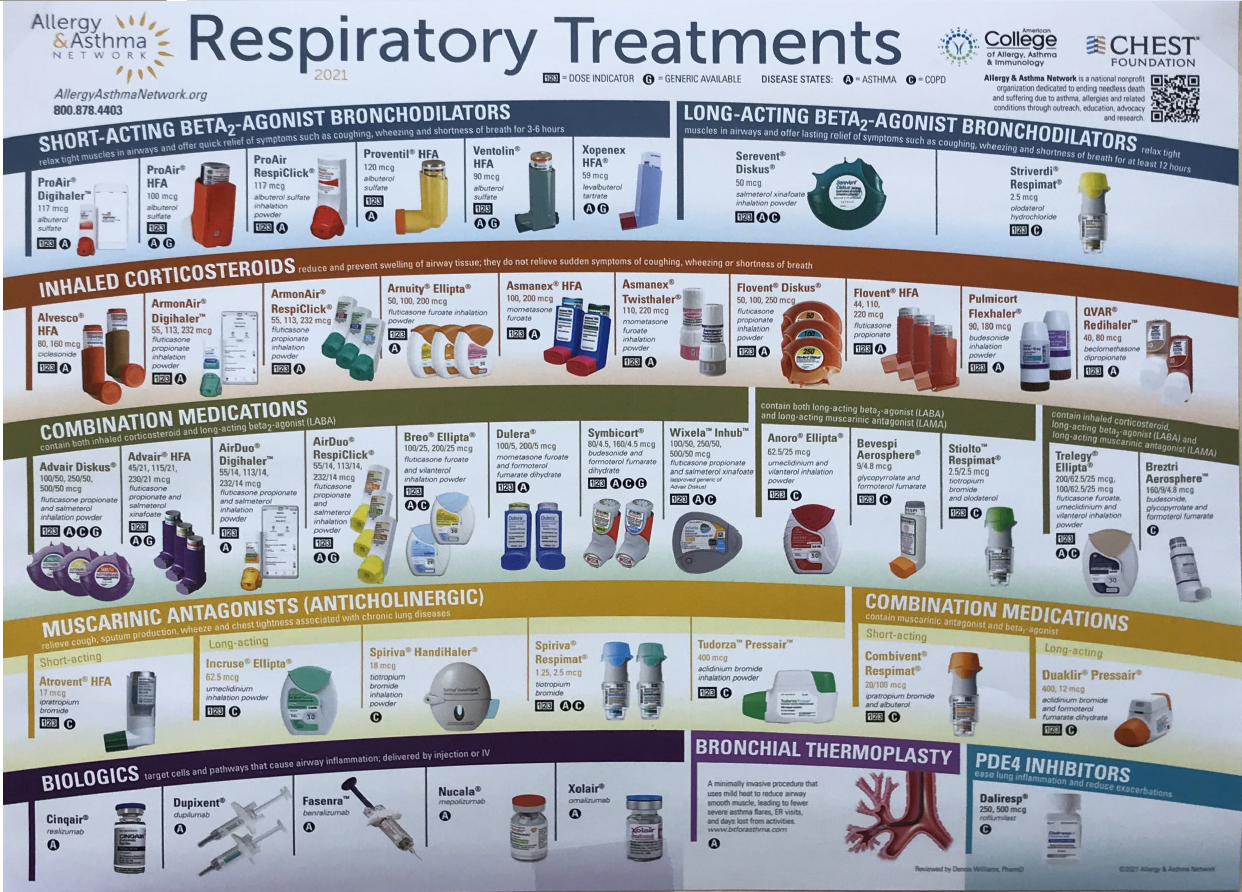
FEV1: FEV stands for forced expiratory volume; FEV1 is a value that can be used to evaluate pulmonary function, determined by the amount of forced expiratory volume in the first second of expiration.
FVC: Stands for forced vital capacity, which is a measure of the total amount of air that can be expired after a maximal inspiration.
Clinical Approach
Epidemiology
As the third leading cause of death in the United States, COPD affects more than 5% of the adult population. COPD is defined as airway obstruction that is not fully reversible, is usually progressive, and is associated with chronic bronchitis, emphysema, or both. The most common etiology is cigarette smoking, which is associated with 80% to 90% of cases of COPD. Other etiologies of COPD include passive exposure to cigarette smoke (“secondhand smoke”) and occupational exposures to dusts (including mining, cotton, silica, and plastics); chemicals; and fumes (eg, welding, heavy metals). Patients with symptoms of COPD who do not smoke or work in high-risk occupations warrant further evaluation. A rare cause of COPD is a genetic deficiency in alpha-1 antitrypsin, which is more common in Caucasians and should be considered when emphysema develops at younger ages (< 45 years of age), especially in nonsmokers.
Pathophysiology
Chronic obstructive pulmonary disease is a disease of inflammation of the airways, lung tissue, and vasculature. Pathologic changes include mucus gland hypertrophy with hypersecretion, ciliary dysfunction, destruction of lung parenchyma, elastin fiber destruction, and airway remodeling. These changes result in a narrowing of the airways, causing a fixed airway obstruction, poor mucus clearance, cough, wheezing, dyspnea, and a predisposition to lung infection.
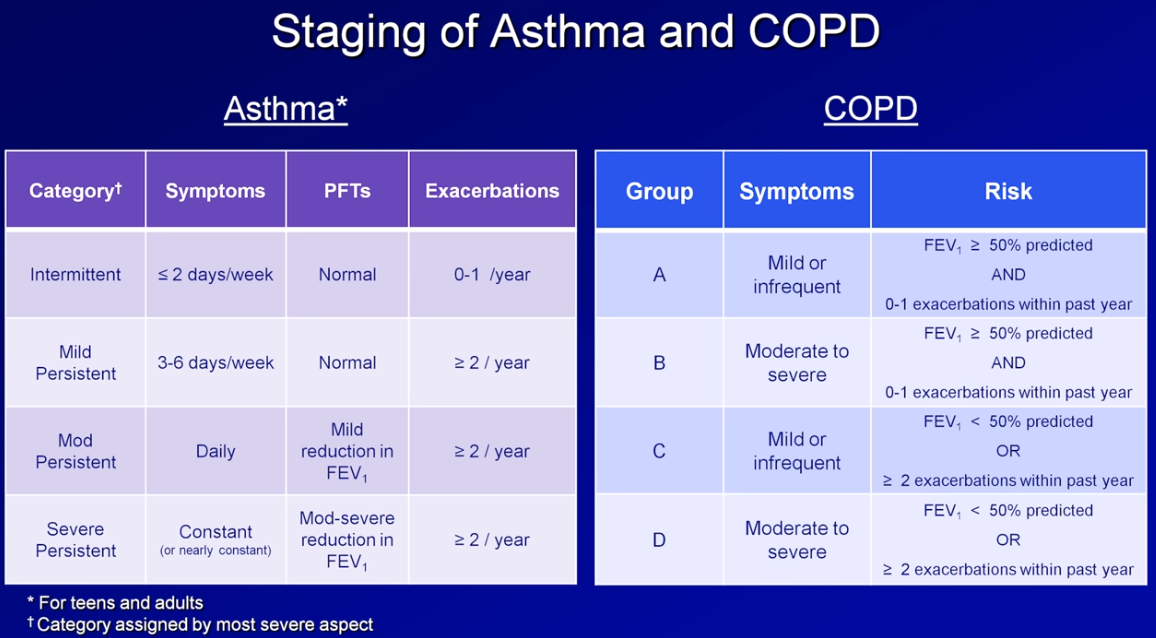
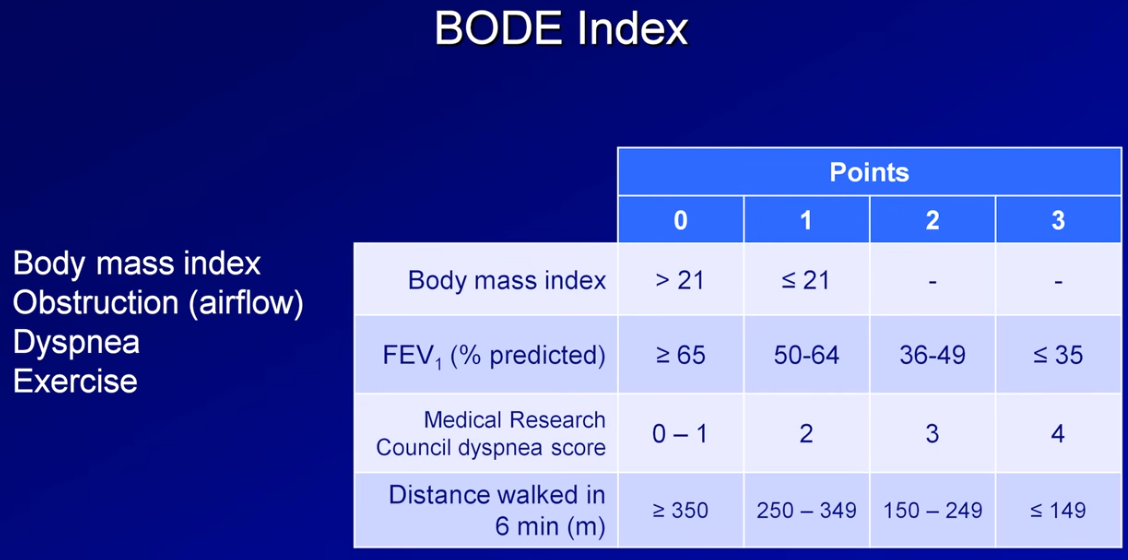
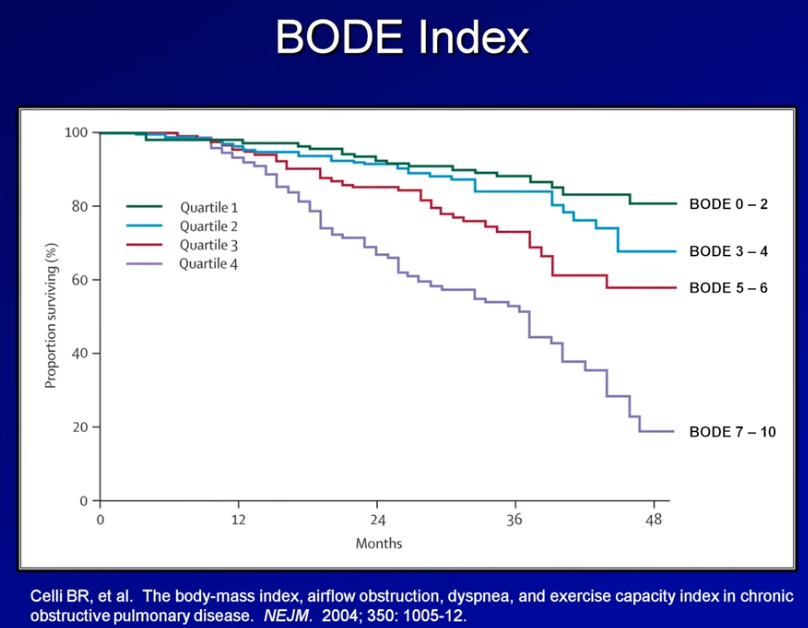
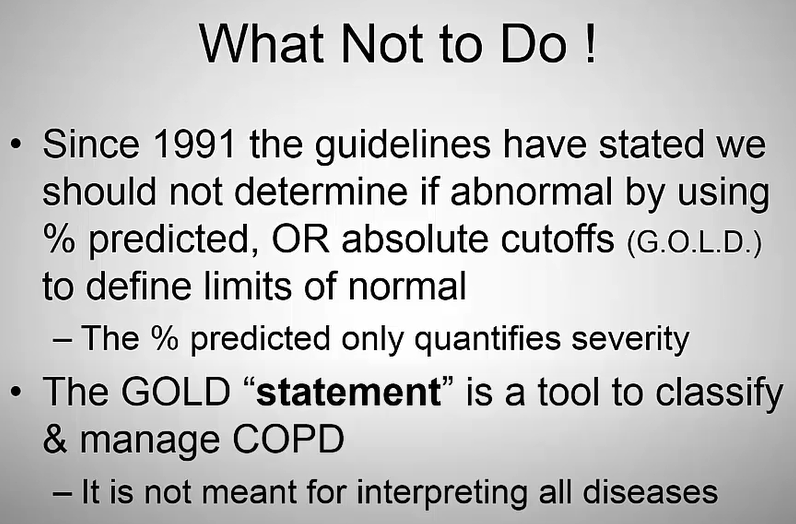
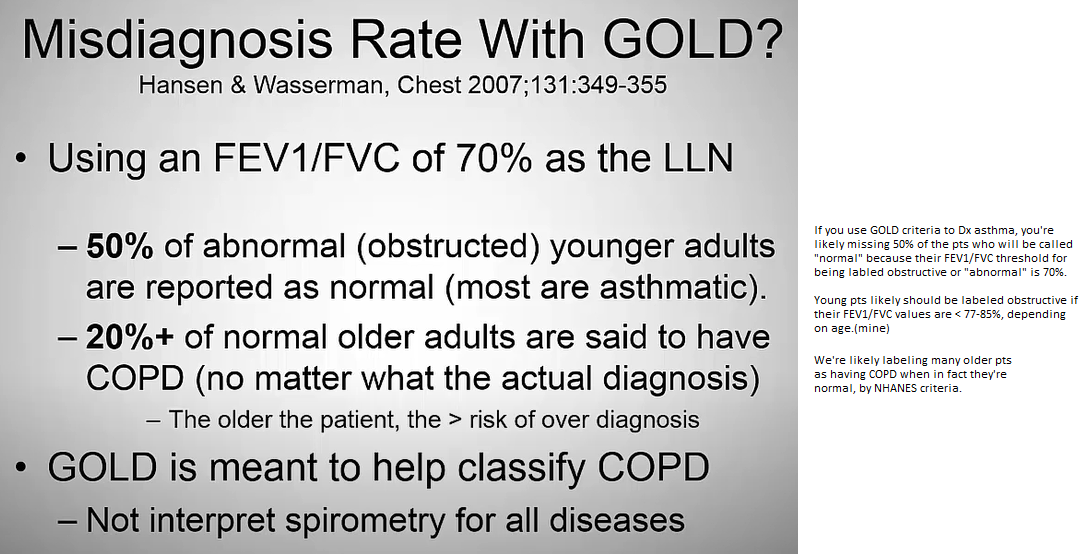
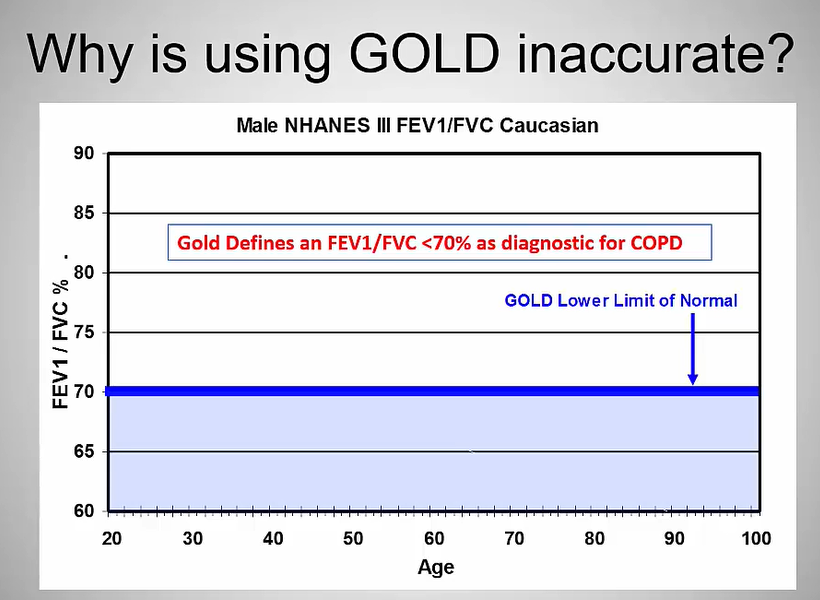
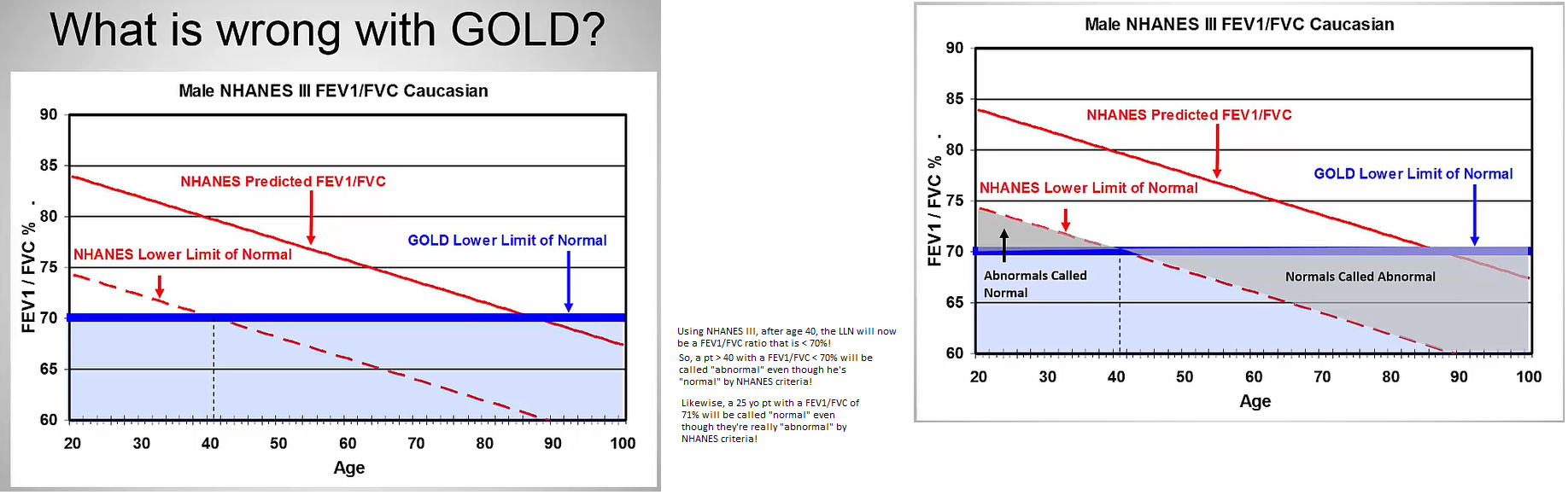
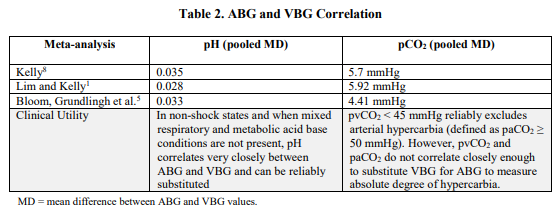
The primary diagnostic test of lung function is spirometry. In normal aging, both the FVC and FEV1 reduce gradually and proportionally over time. In normal-functioning lungs, the ratio of the FEV1 to FVC is greater than 0.7. In COPD, both the FVC and FEV1 are reduced, and the ratio of FEV1 to FVC is less than 0.7, indicating an airway obstruction. Reversibility is defined as an increase in FEV1 of greater than 12% or 200 mL with use of a short-acting bronchodilator. Using a bronchodilator may result in some improvement of both FVC and FEV1, but neither will return to normal, making the diagnosis of a fixed obstruction. The severity of COPD, which can help to determine treatment, can be assessed using measurements established by National Institute of Health and Care Excellence and Global Initiative for Chronic Obstructive Lung Disease (see Table 2–1).
CLASSIFICATION OF COPD SEVERITY
Table 2–1CLASSIFICATION OF COPD SEVERITYView Table|
Favorite Table
|Download (.pdf)
Clinical Presentation
The most common initial symptom of COPD is cough, which is at first intermittent and then frequently becomes a daily occurrence. The cough is often productive with white, thick mucus. Patients will present with intermittent episodes of worsening cough, with change in mucus from clear to yellow/green, and often with wheezing. These exacerbations are usually caused by infection.
As COPD progresses, lung function continues to deteriorate and dyspnea develops. Dyspnea is the primary presenting symptom of COPD. Dyspnea also tends to worsen over time—initially, the dyspnea will occur only with significant effort, then with any exertion, and finally at rest. By the time dyspnea develops, lung function (as measured by FEV1) has been reduced approximately by half, and the COPD has been present for years. When evaluating the patient with dyspnea, it is important to consider other diagnoses. Keep in mind that 85% of dyspnea causes are one of the following conditions: congestive heart failure, COPD, asthma, interstitial lung disease, pneumonia, and psychogenic disturbances (including anxiety).
Examination of a patient with mild or moderate COPD who is not having an exacerbation is usually normal. As the disease progresses, patients are often noted to have “barrel chests” (increased AP chest diameter) and distant heart sounds caused by hyperinflation of the lungs. Breath sounds may also be distant, and expiratory wheezes with a prolonged expiratory phase of respiration may be noted. In late stages, they may develop muscle wasting and cachexia. During an acute exacerbation, patients often appear anxious and tachypneic; they may be using accessory muscles of respiration, usually have wheezes or rales, and may have signs of cyanosis.
Chest x-rays in patients with COPD are typically normal until the disease is advanced. In more severe cases, hyperinflation of the lungs with an increased posteroanterior diameter and flattening of diaphragms may be seen. Bullae—areas of pulmonary parenchymal destruction—can also be seen in x-rays in more severe disease.
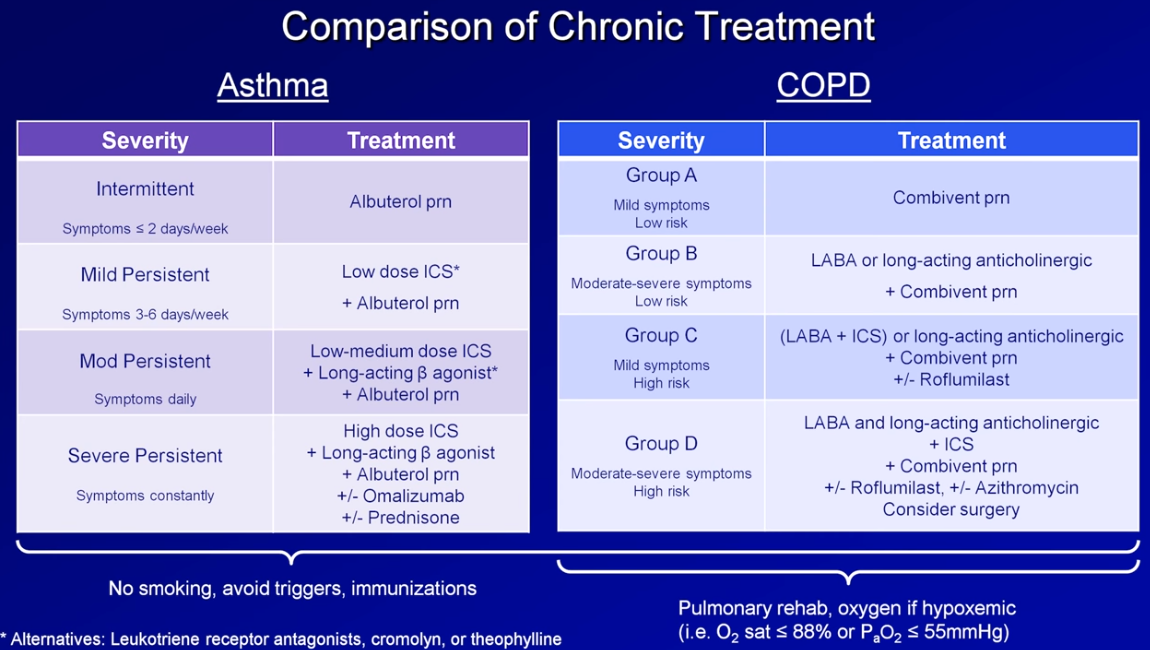
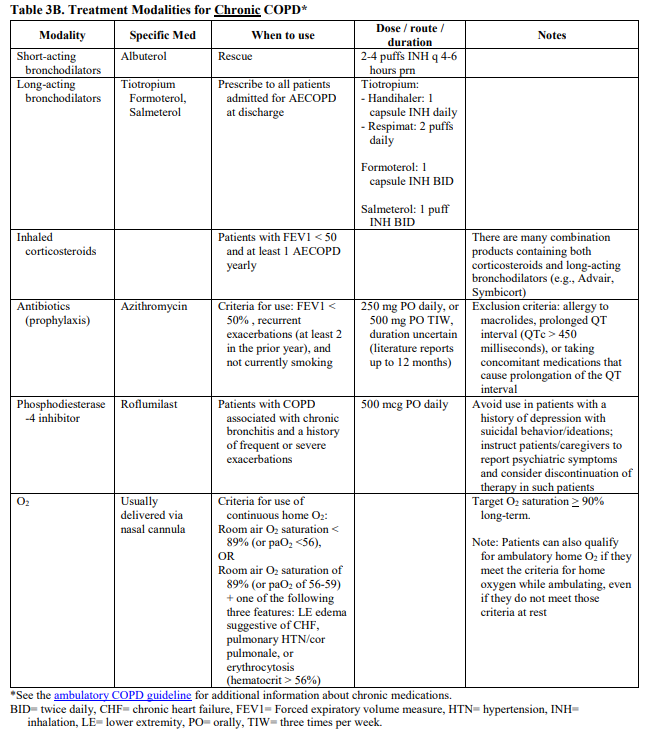
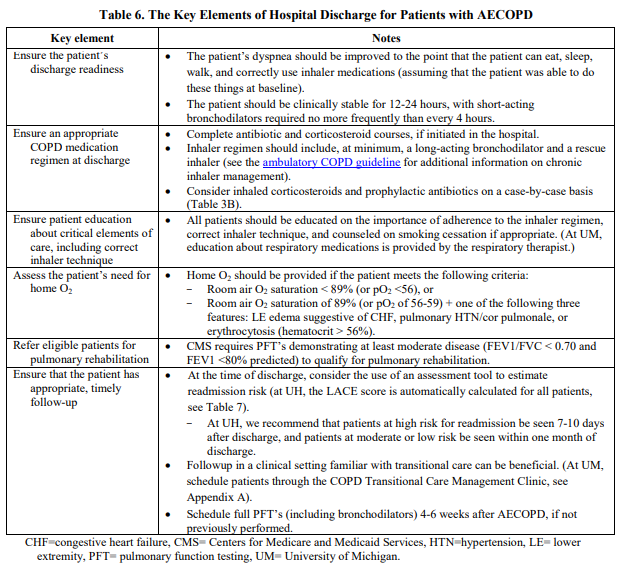
Treatment of Stable COPD
Goals. The goals of COPD management are to relieve symptoms; prevent or slow disease progression; reduce and manage exacerbations; reduce, prevent, and treat complications; and prevent or reduce the frequency of hospitalizations. Several components of treatment are common to all stages of COPD, whereas pharmacologic treatment is guided by the stage of disease.
Smoking Cessation. All patients with COPD should be encouraged to quit smoking. The pulmonary function of smokers declines more rapidly than that of nonsmokers. Although smoking cessation does not result in significant improvement in pulmonary function, smoking cessation does reduce the rate of further deterioration to that of a nonsmoker. Cessation also reduces the risks of other comorbidities, including cardiovascular diseases and cancers. Case 7 more thoroughly discusses smoking cessation. All patients with COPD should be appropriately vaccinated, with both pneumococcal vaccination and annual influenza vaccination. Avoidance of secondhand smoke, aggravating occupational exposures, and indoor and outdoor pollution is recommended.
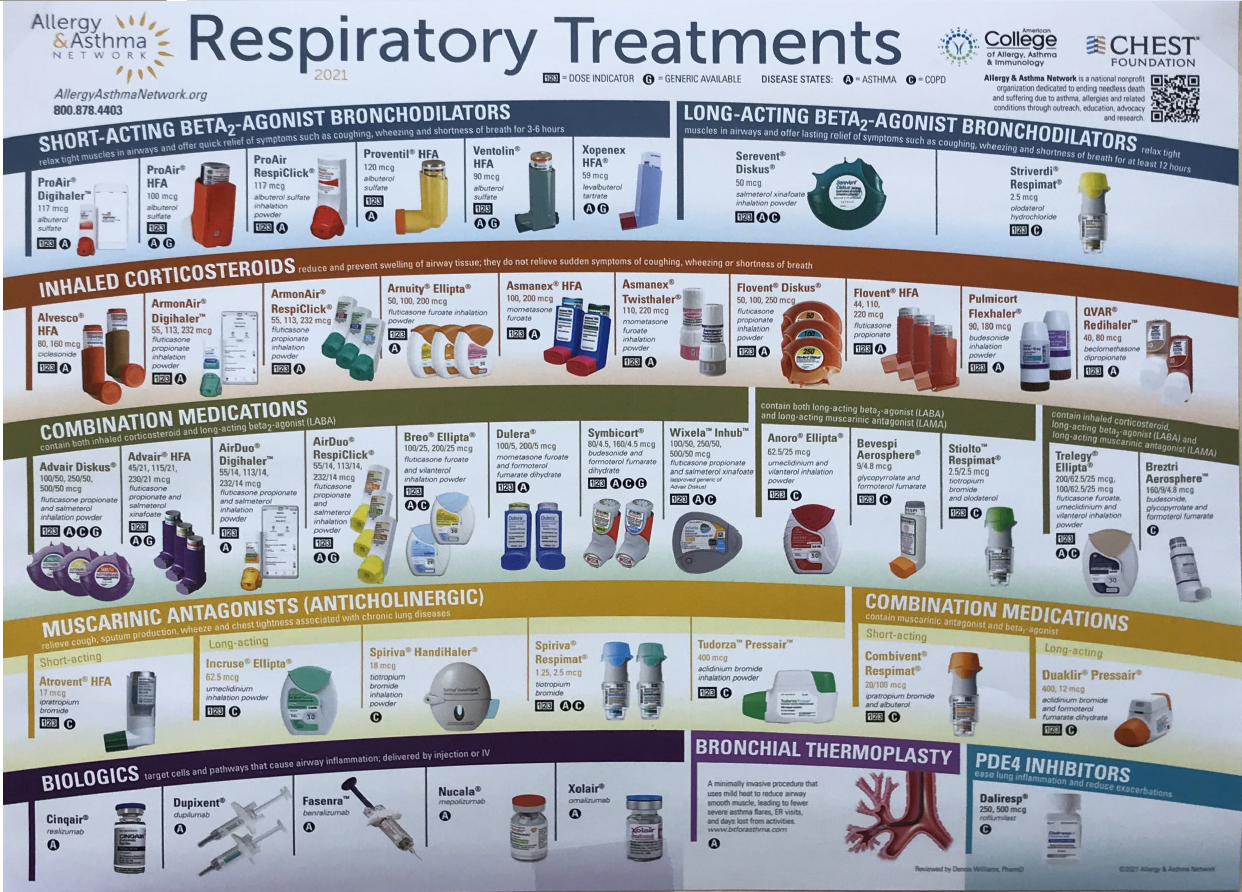
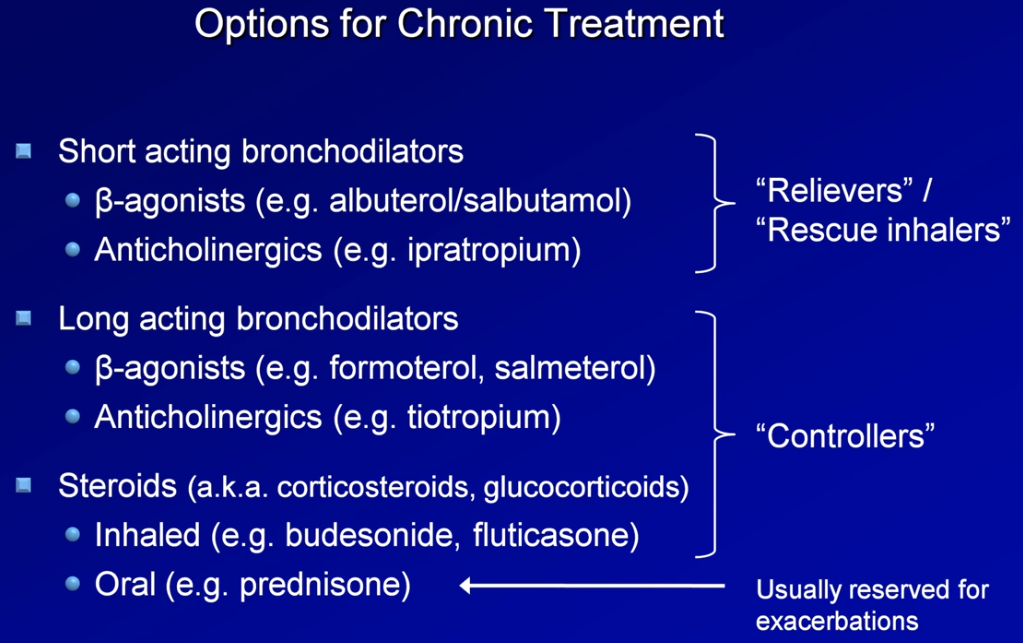
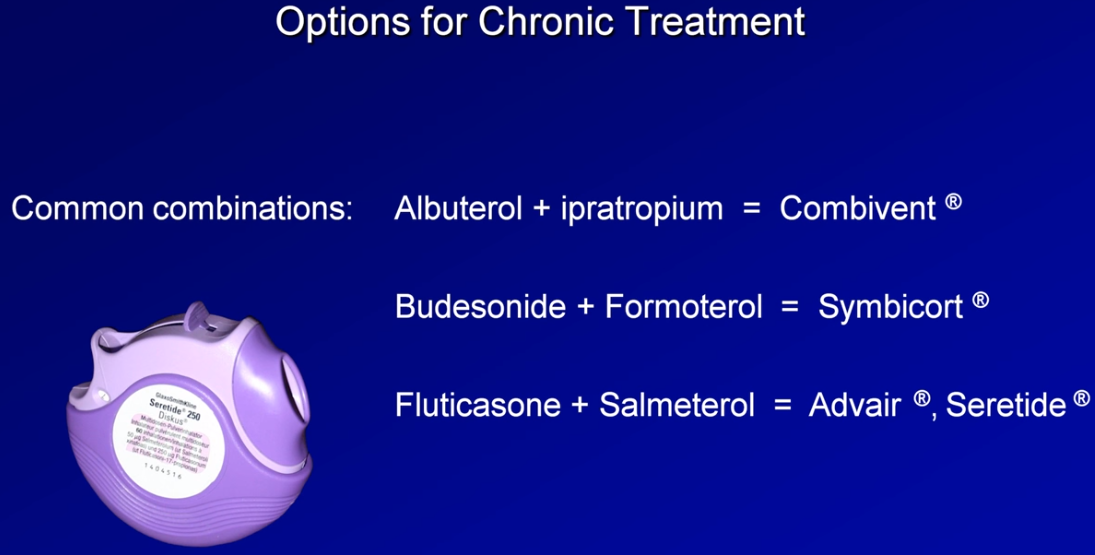
Short-acting Bronchodilators. Although pharmacological treatment cannot reverse lung changes or modify long-term decline in lung function, it does reduce the severity of symptoms, decrease the frequency of exacerbations, decrease hospitalizations, and improve exercise tolerance and overall health. Short-acting bronchodilators used as needed are the recommended treatment in mild COPD. These include beta-2 agonists (albuterol) and anticholinergics (ipratropium). Inhaled medications are preferred due to their fewer side effects. The choice of specific agent is based on availability, individual response to therapy, and side effects.
Long-acting Bronchodilators. In moderate COPD, a long-acting bronchodilator should be added. Commonly used agents in the United States are salmeterol (an inhaled beta-2 agonist) and tiotropium (a long-acting inhaled anticholinergic). Oral methylxanthines (aminophylline, theophylline) are also options but have narrow therapeutic windows (high toxicity) and multiple drug-drug interactions, making their use less common. The use of long-acting bronchodilators is more convenient and more effective than using short-acting agents but is much more expensive and does not replace the need for short-acting agents for rescue therapy in exacerbations.
Steroids. Inhaled steroids (fluticasone, triamcinolone, mometasone, etc) do not affect the rate of decline of lung function in COPD but do reduce the frequency of exacerbations. For that reason, inhaled steroids are recommended for stages severe and very severe COPD with frequent exacerbations. Long-term treatment with oral steroids is not recommended because there is no evidence of benefit and because there can be multiple complications (myopathy, osteoporosis, glucose intolerance, etc). Although continuous prophylactic antibiotic use decreases the number of COPD exacerbations for a few years, there is no decrease in mortality, and the risk of antibiotic resistance makes this a controversial issue.
Oxygen. Oxygen therapy is recommended in very severe COPD if there is evidence of hypoxemia (PaO2 ≤ 55 mm Hg or SaO2 [arterial oxygen saturation] ≤ 88% at rest). Oxygen can also be used if the SaO2 is < 90% and there is polycythemia pulmonary hypertension or peripheral edema suggesting heart failure. Oxygen therapy is the only intervention that has been shown to decrease mortality and must be worn for at least 15 h/d. Depending on the stage of the patient’s COPD, pulmonary rehabilitation and possibly lung resection surgery should be considered with the appropriate specialists when pharmacologic therapy is not providing improvement.
Follow-up. Since COPD is a chronic condition that is expected to worsen over time, routine follow-up is imperative. Spirometry is the best method to monitor lung function. The COPD Assessment Test (CAT) is a questionnaire given to patients every 3 months. The CAT is an objective tool to assess changes over time and the impact that COPD is having on a patient’s life (it can be found at https://www.catestonline.org/).
Treatment of COPD Exacerbations
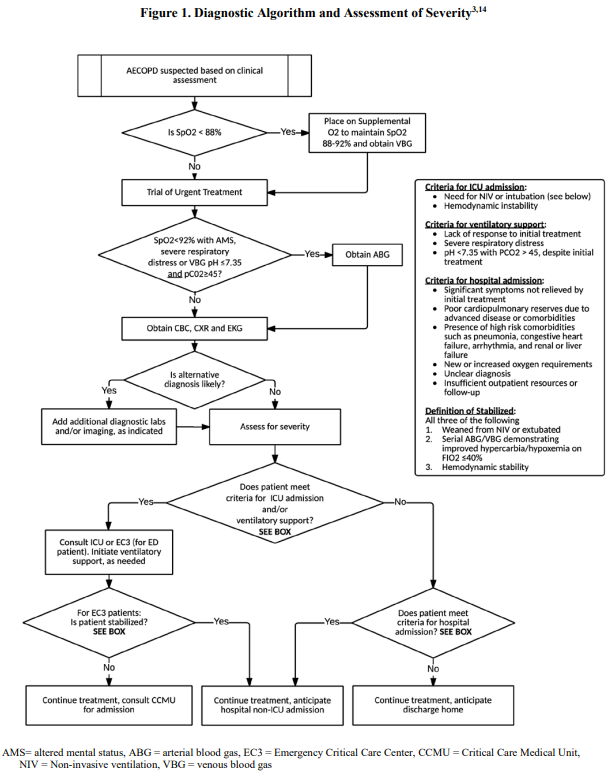
Definition. An acute COPD exacerbation is defined as a change in respiratory function causing worsening of symptoms, which leads to a change in medication. Acute exacerbations of COPD are common & typically present with change in sputum color or amount, cough, tachypnea, wheezing, & increased dyspnea. Although respiratory tract infections (viral and bacterial) are the most common precipitants, air pollutants are another common cause of acute COPD exacerbations. Diagnoses that can cause similar symptoms (eg, pulmonary embolism, CHF, MI, pneumonia, pneumothorax, pleural effusion) must be excluded so that appropriate therapy can occur.
Evaluation. The severity of the exacerbation should be evaluated by history, exam, assessment of oxygenation using pulse oximetry, & focused testing. The following questions from the medical history may help to assist in assessing the exacerbation: number of previous episodes & hospitalizations, other chronic conditions, current treatment regimen, history of intubation/mechanical ventilation, & duration of new symptoms. Signs of severity on physical exam include respiratory rate, use of respiratory muscles, worsening or new cyanosis, unstable blood pressure and heart rate, altered mental status, and peripheral edema. Oxygen should be given with a target saturation of 88% to 92% or PaO2 levels above 60 mm Hg.
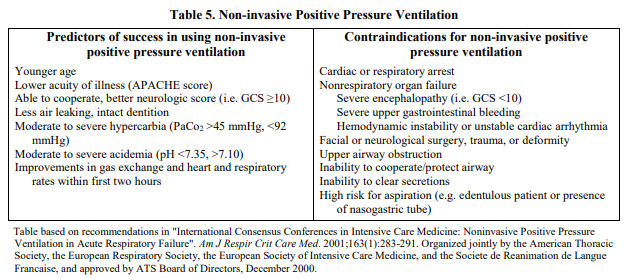
Hospitalization. Patients with more severe symptoms, comorbidities, altered mental status, an inability to care for themselves at home, or whose symptoms fail to respond promptly to office or emergency department treatments should be hospitalized. If hospitalized, a baseline arterial blood gas should be considered to evaluate for hypercapnia, hypoxemia, & respiratory acidosis. Ventilatory support with either noninvasive (nasal or face mask) or invasive (intubation) ventilation should be considered in deteriorating or critical patients.
Bronchodilators and Steroids. All acute exacerbations should be treated with short-acting bronchodilators. Combinations of short-acting agents with different mechanisms of action (ie, beta-2 agonist and anticholinergic) can be used until symptoms improve. Systemic steroids shorten the course of the exacerbation and may reduce the risk of relapse. A steroid dose of 40 mg prednisolone (or equivalent) for 10 to 14 days is recommended.
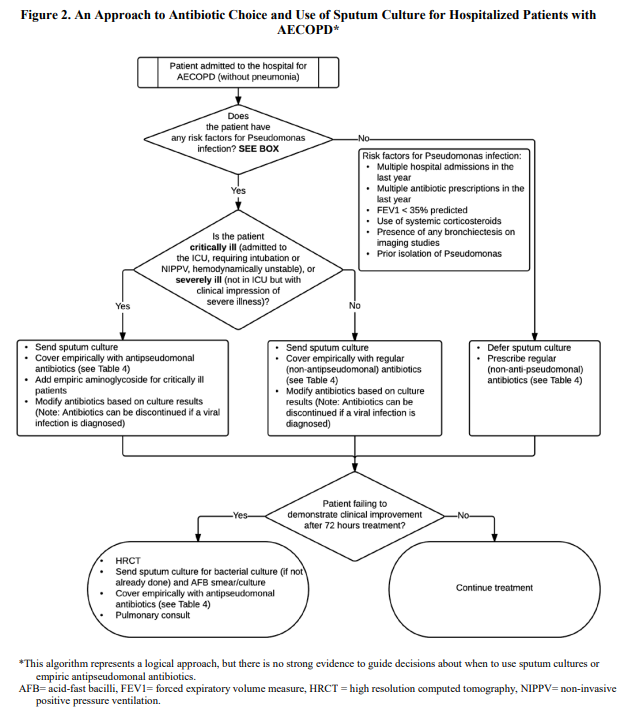
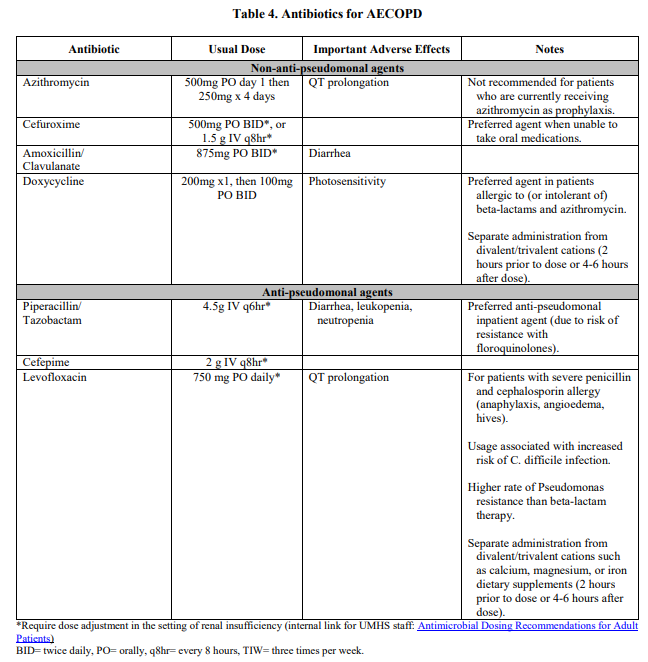
Antibiotics. Exacerbations associated with increased amounts of sputum or with purulent sputum should be treated with antibiotics. A sputum culture should be performed. Pneumococcus, Haemophilus influenzae, and Moraxella catarrhalis are the most common bacteria implicated. In milder exacerbations, treatment with oral agents directed against these pathogens is appropriate. In severe exacerbations, gram-negative bacteria (Klebsiella, Pseudomonas, or other gram-negatives) can also play a role, so antibiotic coverage needs to be broader.
Prevention. Measures taken to prevent COPD exacerbation should be discussed and reviewed at each patient encounter. The number of annual exacerbations can be reduced by receiving appropriate vaccinations (influenza and pneumococcal), smoking cessation counseling, and education about current medications and their proper use. Patients should be encouraged to discuss social concerns, psychiatric problems (eg, anxiety), and proper nutrition and exercise with their provider.
All smokers should be counseled on the benefits of smoking cessation before they develop symptomatic COPD; by the time symptoms develop, the patient’s FEV1 will have been reduced by approximately 50%.
COPD is one of the leading causes of morbidity and mortality.
Always remember to evaluate the ABCs—Airway, Breathing, Circulation—when evaluating a dyspneic patient.
All acute exacerbations should be treated with short-acting bronchodilators.
The primary diagnostic test for COPD is spirometry; a fixed FEV1/FVC ratio < 0.7 is diagnostic.
Oxygen therapy is recommended in very severe COPD if there is evidence of hypoxemia.
QA
A 38-year-old woman presents with progressively worsening dyspnea & cough. She has never smoked cigarettes, has no known passive smoke exposure, and does not have any occupational exposure to chemicals. She has a family history of cirrhosis. Pulmonary function testing shows obstructive lung disease that does not respond to bronchodilators, and a complete metabolic panel demonstrates elevation of alanine aminotransferase (ALT) and aspartate aminotransferase (AST). Which of the following is the most likely etiology?
A Radon exposure at home
B Neoplasm
C Alpha-1 antitrypsin deficiency
D Pulmonary hypertension
Ans: C. This patient has a fixed airway obstruction consistent with COPD. The most common cause of COPD by far is cigarette smoke (90%). Other etiologies include other environmental exposures, such as air pollutants. Alpha-1 antitrypsin deficiency should be considered in a patient who develops COPD at a young age; this condition is also associated with liver dysfunction and can cause cirrhosis. Answer A (radon exposure at home) is a very rare cause of COPD and not as common as alpha-1 antitrypsin deficiency. Answer B (neoplasm) is associated with cough, especially with bloody sputum, weight loss, and cigarette smoking. Pulmonary hypertension (answer D) would not be associated with an obstructive lung disease but presents with progressive dyspnea.
A 60-year-old man is diagnosed with moderately severe COPD. He admits to a long history of cigarette smoking and is still currently smoking one pack per day. In counseling him about the benefits of smoking cessation, which of the following statements is most accurate?
A By quitting, his pulmonary function will significantly improve.
B By quitting, his current pulmonary function will be unchanged, but the rate of pulmonary function decline will slow.
C By quitting, his current pulmonary function and the rate of decline are unchanged, but there are cardiovascular benefits.
D By quitting, his age-related decline in pulmonary function will slow but will not approach that of a nonsmoker of the same age.
Ans: B. By stopping smoking, an individual’s ongoing deterioration of pulmonary function will slow (the rate of decline); unfortunately, the lung damage that has occurred is not affected. Smoking cessation will not result in reversal of the lung damage that has already occurred (answer A). Answer C (cardiovascular benefits but no change in rate of pulmonary decline) is not correct since there the rate of decline does indeed slow. In fact, smoking cessation can result in the rate of decline returning to that of a nonsmoker (answer D).
A 68-year-old patient with known COPD has been having frequent exacerbations of his COPD. Pulmonary function testing shows a FEV1 of 40% predicted (normal = 80% to 120%). His SaO2 by pulse oximetry is 91%. Which of the following medication regimens is the most appropriate at this time?
A Inhaled salmeterol twice daily and albuterol as needed
B Oral albuterol daily and inhaled fluticasone twice daily
C Inhaled fluticasone twice daily, inhaled tiotropium twice daily, and inhaled albuterol as needed
D Inhaled fluticasone twice daily, inhaled tiotropium twice daily, inhaled albuterol as needed, and home oxygen therapy
Ans: C. This patient has severe COPD with frequent exacerbations based on his FEV1 and history. His FEV1 is only 40% and SpO2 is 91%. He is best treated by a long-acting bronchodilator (eg, tiotropium) and an inhaled steroid (eg, fluticasone) used regularly, along with an inhaled, short-acting bronchodilator on an as-needed basis. He does not need long-term oxygen at this point since his SpO2 is not below 88% (answer D). Answer A (inhaled salmeterol and albuterol as needed) would be sufficient for a patient with moderate disease (FEV1 between 50% and 80%). Similarly, answer B (oral albuterol, which is a short-acting bronchodilator, and fluticasone, a long-acting inhaled corticosteroid) is insufficient for severe COPD.
A 59-year-old man with a known history of COPD presents with worsening dyspnea. On examination, he is afebrile. His breath sounds are decreased bilaterally. He is noted to have jugular venous distension (JVD) and 2+ pitting edema of the lower extremities. Which of the following is the most likely cause of his increasing dyspnea?
A COPD exacerbation
B Pneumonia
C Cor pulmonale
D Pneumothorax
Ans: C. JVD & lower extremity edema are suggestive of cor pulmonale, which is right heart failure due to chronically elevated pressures in the pulmonary circulation. Right heart failure causes increased right atrial pressures and right ventricular end-diastolic pressures, which then lead to liver congestion, jugular venous distension, and lower extremity edema. Answer A (COPD exacerbation) usually presents with dyspnea and cough without heart failure. Answer B (pneumonia) is associated with fever, cough, and dyspnea without right heart failure. Answer D (pneumothorax) may be associated with JVD due to increased intrathoracic pressure, but not pedal edema; also, the patient usually has chest pain.
Visit the Asthma vs COPD page here
A bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration. In this case, there was an improvement of 25% (and 810 mL) [math: 4000 mL – 3190 mL = 810 mL] in the FVC and 30% (and 650 mL) [math: 2830 mL – 2180 mL = 650 mL] in the FEV1 so the patient would be classified as having a bronchodilator response.
The presence of a bronchodilator response can be used to support a diagnosis of asthma in the right clinical setting since the hallmark of that disorder is reversible airflow obstruction and the presence of a bronchodilator response demonstrates some evidence of reversibility.
Patient is a XX year-old Navy Recruit referred to Pulmonary Recruit Asthma Clinic for assessment for possible asthma.
Patient denies recent episodes of upper respiratory tract infection or other illnesses.
Patient denies has history of hay fever or seasonal allergies.
Has taken no antihistamines within the past 72 hours, no beta-agonist bronchodilators within the past 8 hours and has not been on any inhaled or oral corticosteroids within the past 14 days.
Patient denies having been was diagnosed with asthma as a child. Patient was told he had asthma at age:
Patient denies ever using a bronchodilator inhaler. Last bronchodilator used was xxxx.
Denies aspirin intolerance.
Previous Medical History: non-contributory
Previous Surgical History: denies sinus surgery
Social History:
Cigarettes: smokes XX cigarettes packs per day for XX years
Vaping: Denies
Family History:
Denies asthma history or history of allergy/atopy. Brother Sister with asthma
Allergies: NKDA
Medications: None
Review of Systems
Denies: shortness of breath, wheezing, cough.
Denies having triggers of wheezing or SOB from: dry air, cold air, exercise, cooking, chemicals, detergents.
Denies having a history of colds that persist 6-8 weeks.
Physical Exam:
HEENT: no nasal polyps
Heart: S1, S2 normal, regular rate and rhythm; no murmurs, rubs or gallops
Chest: normal
Lungs: clear to auscultation bilaterally wheezes (expiratory) heard at
No coughing after deep inspirations/expirations on lung exam.
Extremities: no clubbing or peripheral edema
Test Results
Spirometry(xx/xx/2020): FEV1: (xx%) FVC: (xx%) FEV1/FVC = DLCO: normal
Pre- and post-bronchodilator response was: xx 12% and xx 200 mL
Methacholine Challenge Test: PC20 at xxx mg/mL, patient had a maximum change of (- xx %) -- which is a NORMAL negative (abnormal) positive test.
Exercise Bronchoprovocation Test showed: 10% decrease in FEV1
Assessment:
WEDNESDAY, Jan. 27, 2021 (HealthDay News) -- For patients hospitalized with COVID-19, respiratory, physical, and psychological sequelae are common at four months after discharge, according to a study published online Jan. 27 in JAMA Network Open.
Mattia Bellan, M.D., Ph.D., from the Università del Piemonte Orientale in Novara, Italy, and colleagues examined the prevalence of lung function anomalies, exercise function impairment, and psychological sequelae at four months after discharge among patients aged 18 years and older with confirmed severe acute respiratory syndrome coronavirus 2 infection serious enough to require hospital admission. Data were included for 238 patients.
The researchers found that diffusing lung capacity for carbon monoxide was reduced to less than 80% and less than 60% of the estimated value in 51.6 and 15.5 % of patients, respectively. In 53 patients (22.3 percent), the Short Physical Performance Battery (SPPB) score suggested limited mobility (score <11). Patients with SPPB scores within reference range underwent a two-minute walk test; 75 patients (40.5 percent) had a score outside reference ranges for expected performance. Based on these findings, 128 patients (53.8 percent) had functional impairment. Forty-one patients (17.2 percent) had posttraumatic stress symptoms.
"A significant proportion of patients hospitalized for COVID-19 still reported a high proportion of symptoms associated with COVID-19 up to four months after hospital discharge, with reduced exercise tolerance being the most common," the authors write. "Other midterm sequelae of COVID-19, such as respiratory and physical functional impairment, may impact psychological health."
Unlikely to be asthma given history and physical exam. Normal spirometry--further pulmonary testing not indicated at this time.
[A bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration.]
Spirometry was performed. Good patient effort and cooperation. The test appears to meet the American Thoracic Society standards for acceptability and repeatability.
SPIROMETRY: Flow volume loop appears concave. FVC normal. FEV1 lower limit of normal. FEV1/FVC lower limit of normal. FEF25-75% mildly decreased. Following bronchodilator, there is significant improvement in FEV1 and FEF25-75%.
INTERPRETATION: Mild lower airway obstruction with significant bronchodilator response. Joseph2466-2016
COVID-19 infection. Sxs may persist 4-6 months after Dx. As such, she may need more time to re-condition in order to optimize her chances of passing her PFA.
s/p COVID-19 infection ~ 1.5 months ago. Sxs of fatigue/SOB may persist 4-6 months after Dx. As such, she may need more time to re-condition in order to optimize her chances of passing her PFA. Normal spirometry. Lung Volumes showed slightly decreased TLC with normal diffusion capacity.
Has clinical asthma despite post-BD testing showing normal responses. Recommend ELMS.
Unlikely to be asthma. Normal spirometry. Post-BD testing not indicated. Likely deconditioning.
here for f/u MCT to assess for asthma. Referred by East campus clinics.
Unlikely asthma by history and clinical data. Normal spirometry. Bronchodilator response is not suggestive of asthma. His low FEV1/FVC precludes MCT/EIB today. If still a concern, can send him back for repeat PFTs to see if we can do a MCT on him.
Normal PFTs. Pt s/p asymptomatic Covid-19 infection approximately 3 months ago. Denies any functional limitations. Recommend FFFD in her aviation rating.
Spirometry shows decreased FEV1/FVC ratio suggesting obstruction. Abnormal post-BD response suggests reactive airways disease--likely asthma component: a bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration. Pt denies recent illness or URI Sxs or cough. Since he's special physicals, consider methacholine challenge or exercise-induced bronchoprovocation testing. However, pt ststes he doesn't desire to remain in Navy.
Normal spirometry. Unlikely asthma. Bronchodilator response is not suggestive of asthma. Anxiety component likely. Echo/ECG were unremarkable. Chem 7 & CBC & TFTs were unremarkable. Pregnancy test was negative.
FEV1= xxx ( xxx % pred); FVC= xxx ( xxx % pred); FEV1/FVC= xxx ( xxx % pred); TLC: xxx ( xxx %), DLCO(uncorrected): xxx ( xxx %); DL/VA: xxx ( xxx %)
s/p Covid-19 Dx in June 2020. Asymptomatic. Normal spirometry with normal lung volumes and diffusion capacity. FFFD from pulmonary standpoint for aviation.
Unlikely asthma. Bronchodilator response is not suggestive of asthma. If need to rule OUT asthma, consider methacholine challenge or exercise-induced bronchoprovocation testing.
Normal spirometry, but may have ongoing asthma based on clinical history. He states he has some cold weather intolerance (with respect to breathing) and did not play sports in high school because of concern over SOB/wheezing during competition. With medical waivers being granted for asthma and since pt is not undergoing special physicals, recommend no further testing for asthma unless there is a need to rule OUT asthma. Recommend medical waiver for asthma and for pt to carry beta-agonist inhaler when performing physical activities.
Unlikely asthma. Bronchodilator response is not suggestive of asthma. If need to rule OUT asthma, consider methacholine challenge or exercise-induced bronchoprovocation testing. A bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration. As he is not doing special physicals, don't recommend any further pulmonary testing.
Likely asthma. Abnormal (positive) methacholine challenge test. The methacholine challenge test is considered positive if the results show a 20% or greater decrease in the FEV1 or FVC when compared to patient's baseline. A positive test suggests that the pt's airways are "reactive," and a diagnosis of asthma should be considered.
Clinical asthma by history and spirometry. Spirometry demonstrates an obstructive pattern. Although bronchodilator response is technically not suggestive of asthma, his pre-test probability for asthma is very high. He has h/o childhood asthma. He continues to experience wheezing episodes on exertion; he has cold-weather exercise intolerance due to breathing (inspiration). He is sensitive to dog hair. I don't recommend any further pulmonary testing. He should not undergo MCT due to his decreased FEV1/FVC ratio.
Tolerates pets (cats, dogs). Denies cold environment intolerance.
Clinical asthma. Abnormal (positive) methacholine challenge test (markedly abnormal). Recommend ELMS.
Clinical asthma by history. Father with asthma; perfumes bother her breathing; was not able to make track team due to SOB; used inhaler right before bootcamp for SOB; has cold weather intolerance to breathing. Pre-test probability for asthma is very high; so, no further diagnostic testing recommended. I recommend ELMS for asthma even if approved for medical waiver for asthma.
Unlikely to be asthma given history and physical exam. Ran 5K I high school for 3 years without SOB issues or wheezing. Unlikely to have suddenly developed asthma. Normal spirometry--further pulmonary testing not indicated at this time. If SOB or other symptoms recur, can consider further testing.
Not doing special physicals.
Unlikely asthma by clinical history. Likely deconditioning. Spirometry: normal.
Unlikely asthma by history and clinical data. Normal spirometry. Bronchodilator response is not suggestive of asthma. No further pulmonary testing recommended unless his health status changes.
Unlikely to be asthma. Normal spirometry. Post-BD testing not indicated. No coughing after deep inspiratory efforts during lung exam. Recommend FFD from pulmonary standpoint.
Unlikely to be asthma. Normal spirometry. No coughing after deep inspiratory efforts during lung exam. Exercise-induced Bronchoprovocation results are not consistent with a diagnosis of asthma. Recommend FFD.
Asthma likely. Pt had an abnormal bronchodilator response. An abnormal bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration. The presence of a bronchodilator response can be used to support a diagnosis of asthma in the right clinical setting since the hallmark of that disorder is reversible airflow obstruction and the presence of a bronchodilator response demonstrates some evidence of reversibility.
If there is a need to rule OUT asthma, consider methacholine challenge or exercise-induced bronchoprovocation testing.
FEV1= xxxx ( xxx % pred); FVC= xxxx ( xxxx % pred); FEV1/FVC= xxxx ( xxx % pred); post-BD: FEV1= xxxxx (+ xxx %), FVC= xxxx (+ xxxx %);
Here for PFTs for h/o severe pectus excavatum, s/p surgical repair at age 15. Referred by East campus clinics. Undergoing special physicals for HM-ATF.
FEV1= xxx ( xxx % pred); FVC= xxx ( sss % pred); FEV1/FVC= xxx ( xxx % pred); methacholine challenge: max decline in FEV1 was xxx % at xxx mg/mL; max decline in FVC was xxx % at xxx mg/mL.
FEV1= xxx ( xxx % pred); FVC= xxx ( xxx % pred); FEV1/FVC= xxx ( xxx % pred); methacholine challenge: FEV1= xxx , max % was - xxx %.
RV: 1.36 (113%), TLC: 6.34 (104%), FRCpleth: 2.98 (106%). DLCO(uncorrected): 29.7(103%);
FEV1= xxx ( xxx % pred); FVC= xxx ( xxx % pred); FEV1/FVC= xxx ( xxx % pred); RV: xxx (xxx %), TLC: xxx (xxx %), FRCpleth: xxx (xxx %). DLCO(uncorrected): xxx (xxx %);
EIB (bike): at 5 mins [FEV1: xxx(+ xxx %); FVC: xxx(+ xxx %)]; at 10 mins [FEV1: xxxx(+ xxxx %); FVC: xxxxx(+ xxxx %)]; at 15 mins [FEV1: xxx (+ xxx %); FVC: xxx (+ xxx %)]; at 20 mins [FEV1: xxx (+ xxx %); FVC: xxx (+ xxx %)].
Exercise-induced bronchoprovocation test results are NOT consistent with asthma.
Here for PFTs for h/o severe pectus excavatum, s/p surgical repair at age 15. Referred by East campus clinics. Undergoing special physicals for HM-ATF.
Likely exercise-induced bronchospasm/asthma. Pt's low FEV1/FVC ratio of xx % (similar to last spirometry done last week) suggests obstructive pattern and thus increases her risk for adverse events if EIB test is performed or if MCT is performed. Thus, EIB/MCT not recommended as she has signs/symptoms to support a clinical diagnosis of asthma. Recommend ELMS.
Pt left before being seen by me. Pt apparently a Dive candidate/special physicals. Unlikely to be asthma. Pt did not exhibit a significant bronchodilator response. A bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration.If need to rule OUT asthma, consider methacholine challenge or exercise-induced bronchoprovocation testing--when available.
MCCT: FEV1 decreased by 4% max; FVC decreased by max of 3%.
Normal spirometry. Pt had a normal response to the Methacholine Challenge test. Unlikely asthma.
Normal spirometry.
Pt had an abnormal bronchodilator response suggesting a diagnosis of asthma (+22 % post-BD response, > 200mL change). Pt also with sickle cell trait and chest discomfort with extreme exertion. To see Cardiology next. Pt also has (+) TB test, which is being evaluated CXR was read as unremarkable. She denies cough, fever, night sweats, or anorexia/wt loss or travel to TB-endemic areas.
Here for screening for possible asthma. Referred by East Campus.
Unlikely to be asthma per clinical hx and normal spirometry. Post-BD testing not indicated.
Denies cold weather intolerance with respect to SOB.
Pt had an abnormal bronchodilator response suggesting a diagnosis of asthma. A bronchodilator response is defined as a 200 mL and 12% increase in the FEV1 or FVC following bronchodilator administration. The presence of a bronchodilator response can be used to support a diagnosis of asthma in the right clinical setting since the hallmark of that disorder is reversible airflow obstruction and the presence of a bronchodilator response demonstrates some evidence of reversibility. If there is a need to rule OUT asthma, consider methacholine challenge or exercise-induced bronchoprovocation testing.
Needs methacholine challenge test performed. Normal spirometry. Will see him next week in pulm clinic.
methacholine challenge: max % decrease was (-xxx%) on FEV1; max % decrease was (-xxxx%) on FVC.
A test is considered positive if PD20 is <= 200mcg or PC20 is <=8mg/mL. A test is considered negative if PD20 is > 400mcg or PC20 is >16mg/mL. If using SGaw, 100mcg, or 4mg/mL or less indicates a positive test.
Methacholine challenge test: PC20: -xx% at xx mg/mL, which meets the guidelines for being a normal test, ruling out asthma. Pt denies cold environment worsening breathing. He has a h/o seasonal allergies & hay fever per pt.
-bronchoprovocation tests: methacholine challenge test Exercise-induced bronchoprovocation test is NOT consistent with asthma
- unlikely asthma by clinical history. No pulmonary testing recommended as this pt has sickle cell trait which likely explains his symptoms. Data (EST, ECHO) show that his heart function is normal. Recommend entry level medical separation without further testing due to symptoms borne from having sickle cell trait.
Follow up with Recruit Training Command, BHC 1007.
PFT is the gold standard in evaluating alveolar injury compared to spirometry because spirometry can be normal with early or mild disease while PFT will still show low DLCO.
short of breath? wheezing? Do these symptoms come and go?
Patients who are always short of breath probably don’t have asthma! Broaden your differential!
Cough: dry suggests asthma, productive suggests something else
Advising patients to avoid triggers is critical in disease management
Common triggers include: Dry air, cold air, exercise, cooking, chemicals, detergents. These can all lead to bronchospasm!
History of colds that persist 6-8 weeks?
Typical of a URI followed by an asthma exacerbation!
Allergy history: Hay fever? Sinus infections? History of sinus surgeries? Use of allergy medications? Pets? May be the cause for the patient’s symptoms or seen in association with underlying asthma
Acid reflux is very common and may be the cause of the patient’s symptoms or an aggravating factor/trigger.
Physical exam in asthma
General: Obesity? May suggest acid reflux disease
Evaluate neck and mouth (Mallampati Score). Does this person have risk factors for obstructive sleep apnea?
Nasal exam: look for polyps
Lung exam: Listen for cough, expiratory wheeze. Absence of end-expiratory wheezes but cough at the end of deep breaths may be present in cough variant asthma
Look for clubbing, peripheral edema, loud heart murmur. These are important pertinent negatives.
HISTORY OF PRESENT ILLNESS:
--------------------------
Patient referred to Pulmonary Medicine as for the last 1-1.5 months he has been
having SOB and Chest Pain/Pressure with exertion.
Prior to that was able to walk >3-4 miles before needing to stop.
Now he has been gettin SOb and CP with around half that distance.
Symptoms come on much quicker when he runs.
1-2 years ago his father was diagnosed with CAD and had similar symptoms prior
to that and patient is worried about the same.
Usually SOB and CP at the same time or SOb precedes CP by a few minutes, but
always has both.
No symptoms at rest at any time.
No cough at any time.
COPD No
Childhood Asthma: No
Childhood Hay Fever: No
Asthma No
Emergency Intubations: No
Cough today: No
Chronic cough: No
Ever any Hemoptysis: No
Inhalers No
Antihistamine No
Nasal Spray No
Singulair No
Ever Smoker No
Allergies: None known of
Pets: Yes, dogs, no breathing issues around the same
Birds: No
Known mold exposure: No
Known TB exposure: No
Known Asbestos exposure: No
Known chemical/gas/fumes inhalational exposure: No
Second Hand Smoke: No
GERD/Heartburn: No
History of PNA: No
Occupation Recruit
Immunization History
Pneumococcal
Influenza vaccine yearly Yes/No
Last Influenza Vaccine
FAMILY HISTORY
Asthma Yes, sister
Lung Cancer No
Other Lung Problems No
PMH
None
SH
Smoking: As above
Alcohol: None
Drug Use: None
REVIEW OF SYSTEMS
General: No fevers. No chills. No unexplained weight loss recently.
Skin: No itching.
HEENT: No nasal congestion. No nasal discharge.
Cardiovascular: No chest pain. No palpitations.
Respiratory: No SOB. No cough. No wheezing.
Gastrointestinal: No nausea. No vomiting. No constipation. No diarrhea. No
difficulty swallowing.
Extremities: No lower extremity edema.
Neurological: No dizziness. No focal weakness.
Urinary: No dysuria.
Sleep: No daytime sleepiness. No snoring. No waking up coughing/gagging/choking.
ACTIVE MEDICATIONS:
Active Outpatient Medications (excluding Supplies):
No Medications Found
ALLERGIES:
Patient has answered NKA
PHYSICAL EXAMINATION:
Patient is alert,awake and oriented x3 in no acute distress
VITALS:
T 98 F [36.7 C] (06/23/2020 10:25)
BP 118/62 (06/23/2020 10:25)
P 79 (06/23/2020 10:25)
R 14 (06/23/2020 10:25)
BMI [23] on (06/23/20)
SpO2 Measurement DT POx
(L/MIN)(%)
06/23/2020 10:25 97
General: No acute distress.
Lungs: Bilateral breath sounds clear. No wheezing. No rhonchi. No crackles.
Heart: S1S2 present. Regular rate. Regular rhythm.
Abdo: Soft. No tenderness.
Ext: No LE edema.
Neuro: Alert. Moving all 4 ext.
IMAGING:
CXR 05/2020 - No acute abnormality
ASSESSMENT/PLAN:
=================
Dyspnea on Exertion and Associated Chest Pain
Never had PFTs done.
CXR from 05/2020 with no acute abnormality.
No wheezing at any time.
No h/o allergies/hay fever/childhood asthma.
Will check baseline Spirometry and Test for Exercise Induced Bronchospasm,
further recommendations after testing for the same.
Patient's symptoms are always accompanied byChest Pain.
Has been referred to Cardiology as well and is awaiting the consult.
RTC to Clinic in 3 weeks
Sources:
https://www.ncbi.nlm.nih.gov/books/NBK482339/ Pulmonary Function Tests